Cancer Statistics, 2015
Rebecca L. Siegel, MPH1*; Kimberly D. Miller, MPH2; Ahmedin Jemal, DVM, PhD3
Each year the American Cancer Society estimates the numbers of new cancer cases and deaths that will occur in the United States in the current year and compiles the most recent data on cancer incidence, mortality, and survival. Incidence data were collected by the National Cancer Institute (Surveillance, Epidemiology, and End Results [SEER] Program), the Centers for Disease Control and Prevention (National Program of Cancer Registries), and the North American Association of Central Cancer Registries. Mortality data were collected by the National Center for Health Statistics. A total of 1,658,370 new cancer cases and 589,430 cancer deaths are projected to occur in the United States in 2015. During the most recent 5 years for which there are data (2007-2011), delay-adjusted cancer incidence rates (13 oldest SEER registries) declined by 1.8% per year in men and were stable in women, while cancer death rates nationwide decreased by 1.8% per year in men and by 1.4% per year in women. The overall cancer death rate decreased from 215.1 (per 100,000 population) in 1991 to 168.7 in 2011, a total relative decline of 22%. However, the magnitude of the decline varied by state, and was generally lowest in the South (�15%) and highest in the Northeast (�20%). For example, there were declines of 25% to 30% in Maryland, New Jersey, Massachusetts, New York, and Delaware, which collectively averted 29,000 cancer deaths in 2011 as a result of this progress. Further gains can be accelerated by applying existing cancer control knowledge across all segments of the population. CA Cancer J Clin 2015;000:000
C
000. V2015 American Cancer Society.
Keywords: cancer statistics, incidence, trends, survival, mortality, death rates, cancer cases
Introduction
Cancer is a major public health problem in the United States and many other parts of the world. It is currently the second leading cause of death in the United States, and is expected to surpass heart diseases as the leading cause of death in the next few years. In this article, we provide the expected numbers of new cancer cases and deaths in 2015 in the United States nationally and for each state, as well as a comprehensive overview of cancer incidence, mortality, and survival rates and trends using the most current population-based data. In addition, we estimate the total number of deaths averted nationally during the past 2 decades and by state in 2011 as a result of the continual decline in cancer death rates. We also present the actual number of deaths reported in 2011 by age for the 10 leading causes of death and for the 5 leading causes of cancer death.
Materials and Methods
Incidence and Mortality Data
Mortality data from 1930 to 2011 were obtained from the National Center for Health Statistics (NCHS).1 Forty-seven states and the District of Columbia met data quality requirements for reporting to the national vital statistics system in 1930. Texas, Alaska, and Hawaii began reporting mortality data in 1933, 1959, and 1960, respectively. The methods for abstraction and age adjustment of mortality data are described elsewhere.2,3
Population-based cancer incidence data in the United States have been collected by the National Cancer Institute’s (NCI’s) Surveillance, Epidemiology, and End Results (SEER) Program since 1973 and by the Centers for Disease Control and Prevention’s National Program of Cancer Registries (NPCR) since 1995. The SEER program is the only source for long-term, delay-adjusted, population-based incidence data. Long-term incidence and survival trends (1975-2011) were based on data from the 9 oldest SEER areas (Connecticut, Hawaii, Iowa, New Mexico, Utah, and the metropolitan areas of Atlanta, Detroit, San Francisco-Oakland, and Seattle-Puget Sound), representing approximately 9% of the US population.4
1Director, Surveillance Information, Surveillance and Health Services Research, American Cancer Society, Atlanta, GA; 2Epidemiologist, Surveillance and Health Services Research, American Cancer Society, Atlanta, GA; 3Vice President, Surveillance and Health Services Research, American Cancer Society, Atlanta, GA
Corresponding author: Rebecca L. Siegel, MPH, Surveillance and Health Services Research, American Cancer Society, 250 Williams St, NW, Atlanta, GA 30303-1002; Rebecca.siegel@cancer.org
DISCLOSURES: The authors report no conflicts of interest.
doi: 10.3322/caac.21254. Available online at cacancerjournal.com
TABLE 1. Estimated New Cancer Cases and Deaths by Sex, United States, 2015*
| BOTH SEXES | ESTIMATED NEW CASES MALE | FEMALE | BOTH SEXES | ESTIMATED DEATHS MALE | FEMALE | |
|---|---|---|---|---|---|---|
| All sites | 1,658,370 | 848,200 | 810,170 | 589,430 | 312,150 | 277,280 |
| Oral cavity & pharynx | 45,780 | 32,670 | 13,110 | 8,650 | 6,010 | 2,640 |
| Tongue | 14,320 | 10,310 | 4,010 | 2,190 | 1,500 | 690 |
| Mouth | 12,920 | 7,750 | 5,170 | 2,120 | 1,200 | 920 |
| Pharynx | 15,520 | 12,380 | 3,140 | 2,660 | 2,010 | 650 |
| Other oral cavity | 3,020 | 2,230 | 790 | 1,680 | 1,300 | 380 |
| Digestive system | 291,150 | 163,050 | 128,100 | 149,300 | 86,540 | 62,760 |
| Esophagus | 16,980 | 13,570 | 3,410 | 15,590 | 12,600 | 2,990 |
| Stomach | 24,590 | 15,540 | 9,050 | 10,720 | 6,500 | 4,220 |
| Small intestine | 9,410 | 4,960 | 4,450 | 1,260 | 670 | 590 |
| Colon† | 93,090 | 45,890 | 47,200 | 49,700 | 26,100 | 23,600 |
| Rectum | 39,610 | 23,200 | 16,410 | |||
| Anus, anal canal, & anorectum | 7,270 | 2,640 | 4,630 | 1,010 | 400 | 610 |
| Liver & intrahepatic bile duct | 35,660 | 25,510 | 10,150 | 24,550 | 17,030 | 7,520 |
| Gallbladder & other biliary | 10,910 | 4,990 | 5,920 | 3,700 | 1,660 | 2,040 |
| Pancreas | 48,960 | 24,840 | 24,120 | 40,560 | 20,710 | 19,850 |
| Other digestive organs | 4,670 | 1,910 | 2,760 | 2,210 | 870 | 1,340 |
| Respiratory system | 240,390 | 130,260 | 110,130 | 162,460 | 89,750 | 72,710 |
| Larynx | 13,560 | 10,720 | 2,840 | 3,640 | 2,890 | 750 |
| Lung & bronchus | 221,200 | 115,610 | 105,590 | 158,040 | 86,380 | 71,660 |
| Other respiratory organs | 5,630 | 3,930 | 1,700 | 780 | 480 | 300 |
| Bones & joints | 2,970 | 1,640 | 1,330 | 1,490 | 850 | 640 |
| Soft tissue (including heart) | 11,930 | 6,610 | 5,320 | 4,870 | 2,600 | 2,270 |
| Skin (excluding basal & squamous) | 80,100 | 46,610 | 33,490 | 13,340 | 9,120 | 4,220 |
| Melanoma of the skin | 73,870 | 42,670 | 31,200 | 9,940 | 6,640 | 3,300 |
| Other nonepithelial skin | 6,230 | 3,940 | 2,290 | 3,400 | 2,480 | 920 |
| Breast | 234,190 | 2,350 | 231,840 | 40,730 | 440 | 40,290 |
| Genital system | 329,330 | 231,050 | 98,280 | 58,670 | 28,230 | 30,440 |
| Uterine cervix | 12,900 | 12,900 | 4,100 | 4,100 | ||
| Uterine corpus | 54,870 | 54,870 | 10,170 | 10,170 | ||
| Ovary | 21,290 | 21,290 | 14,180 | 14,180 | ||
| Vulva | 5,150 | 5,150 | 1,080 | 1,080 | ||
| Vagina & other genital, female | 4,070 | 4,070 | 910 | 910 | ||
| Prostate | 220,800 | 220,800 | 27,540 | 27,540 | ||
| Testis | 8,430 | 8,430 | 380 | 380 | ||
| Penis & other genital, male | 1,820 | 1,820 | 310 | 310 | ||
| Urinary system | 138,710 | 96,580 | 42,130 | 30,970 | 21,110 | 9,860 |
| Urinary bladder | 74,000 | 56,320 | 17,680 | 16,000 | 11,510 | 4,490 |
| Kidney & renal pelvis | 61,560 | 38,270 | 23,290 | 14,080 | 9,070 | 5,010 |
| Ureter & other urinary organs | 3,150 | 1,990 | 1,160 | 890 | 530 | 360 |
| Eye & orbit | 2,580 | 1,360 | 1,220 | 270 | 140 | 130 |
| Brain & other nervous system | 22,850 | 12,900 | 9,950 | 15,320 | 8,940 | 6,380 |
| Endocrine system | 64,860 | 16,520 | 48,340 | 2,890 | 1,350 | 1,540 |
| Thyroid | 62,450 | 15,220 | 47,230 | 1,950 | 870 | 1,080 |
| Other endocrine | 2,410 | 1,300 | 1,110 | 940 | 480 | 460 |
| Lymphoma | 80,900 | 44,950 | 35,950 | 20,940 | 12,140 | 8,800 |
| Hodgkin lymphoma | 9,050 | 5,100 | 3,950 | 1,150 | 660 | 490 |
| Non-Hodgkin lymphoma | 71,850 | 39,850 | 32,000 | 19,790 | 11,480 | 8,310 |
| Myeloma | 26,850 | 14,090 | 12,760 | 11,240 | 6,240 | 5,000 |
| Leukemia | 54,270 | 30,900 | 23,370 | 24,450 | 14,210 | 10,240 |
| Acute lymphocytic leukemia | 6,250 | 3,100 | 3,150 | 1,450 | 800 | 650 |
| Chronic lymphocytic leukemia | 14,620 | 8,140 | 6,480 | 4,650 | 2,830 | 1,820 |
| Acute myeloid leukemia | 20,830 | 12,730 | 8,100 | 10,460 | 6,110 | 4,350 |
| Chronic myeloid leukemia | 6,660 | 3,530 | 3,130 | 1,140 | 590 | 550 |
| Other leukemia‡ | 5,910 | 3,400 | 2,510 | 6,750 | 3,880 | 2,870 |
| Other & unspecified primary sites‡ | 31,510 | 16,660 | 14,850 | 43,840 | 24,480 | 19,360 |
*Rounded to the nearest 10; estimated new cases exclude basal cell and squamous cell skin cancers and in situ carcinoma except urinary bladder. About 60,290 cases of carcinoma in situ of the female breast and 63,440 cases of melanoma in situ will be newly diagnosed in 2015.
†Estimated deaths for colon and rectum cancers are combined due to a high percentage of misclassification.
‡More deaths than cases may reflect lack of specificity in recording underlying cause of death on death certificates and/or an undercount in the case estimate.
TABLE 2. Estimated New Cases for Selected Cancers by State, 2015*
| ALL | FEMALE | UTERINE | COLON & | UTERINE | LUNG & | MELANOMA | NON-HODGKIN | URINARY | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| STATE | CASES | BREAST | CERVIX | RECTUM | CORPUS | LEUKEMIA | BRONCHUS | OF THE SKIN | LYMPHOMA | PROSTATE | BLADDER |
| Alabama | 26,150 | 3,680 | 230 | 2,150 | 660 | 730 | 4,150 | 1,380 | 1,020 | 3,590 | 1,000 |
| Alaska | 3,700 | 470 | † | 290 | 100 | 110 | 420 | 100 | 140 | 490 | 180 |
| Arizona | 32,440 | 4,750 | 200 | 2,440 | 940 | 950 | 3,740 | 1,400 | 1,300 | 4,090 | 1,580 |
| Arkansas | 15,830 | 2,090 | 150 | 1,420 | 420 | 480 | 2,620 | 360 | 670 | 2,050 | 630 |
| California | 172,090 | 25,270 | 1,490 | 14,510 | 5,800 | 5,970 | 18,430 | 8,560 | 7,870 | 21,060 | 7,150 |
| Colorado | 24,540 | 3,640 | 170 | 1,800 | 740 | 870 | 2,560 | 1,400 | 1,090 | 3,600 | 1,080 |
| Connecticut | 21,970 | 3,190 | 130 | 1,580 | 810 | 660 | 2,870 | 780 | 920 | 3,170 | 1,140 |
| Delaware | 5,280 | 780 | † | 400 | 180 | 160 | 860 | 280 | 220 | 740 | 250 |
| Dist. of Columbia | 2,800 | 430 | † | 230 | 100 | 70 | 310 | 80 | 100 | 490 | 80 |
| Florida | 114,040 | 15,470 | 980 | 9,330 | 3,550 | 3,930 | 16,810 | 5,480 | 5,340 | 15,480 | 5,670 |
| Georgia | 48,070 | 7,170 | 430 | 3,820 | 1,330 | 1,430 | 6,460 | 2,350 | 1,870 | 7,450 | 1,720 |
| Hawaii | 6,730 | 1,140 | 50 | 720 | 280 | 230 | 890 | 420 | 310 | 710 | 220 |
| Idaho | 8,080 | 1,070 | † | 620 | 240 | 300 | 910 | 470 | 380 | 1,270 | 410 |
| Illinois | 65,460 | 9,570 | 550 | 5,720 | 2,470 | 2,200 | 8,920 | 2,380 | 2,890 | 8,140 | 2,970 |
| Indiana | 35,620 | 4,600 | 280 | 2,890 | 1,180 | 1,100 | 5,510 | 1,460 | 1,490 | 4,040 | 1,590 |
| Iowa | 17,140 | 2,390 | 100 | 1,490 | 640 | 640 | 2,440 | 1,070 | 830 | 2,170 | 800 |
| Kansas | 14,440 | 2,130 | 90 | 1,080 | 500 | 480 | 1,930 | 850 | 640 | 1,860 | 620 |
| Kentucky | 26,490 | 3,300 | 220 | 2,090 | 730 | 820 | 4,680 | 1,530 | 1,030 | 3,040 | 1,070 |
| Louisiana | 24,100 | 2,900 | 220 | 2,150 | 570 | 690 | 3,380 | 540 | 950 | 3,980 | 910 |
| Maine | 8,810 | 1,010 | 50 | 610 | 340 | 320 | 1,360 | 320 | 390 | 1,100 | 540 |
| Maryland | 30,050 | 4,730 | 230 | 2,360 | 1,080 | 780 | 3,980 | 1,410 | 1,230 | 4,620 | 1,250 |
| Massachusetts | 37,790 | 5,890 | 210 | 2,550 | 1,460 | 1,130 | 5,150 | 1,310 | 1,620 | 5,420 | 2,000 |
| Michigan | 57,420 | 7,780 | 350 | 4,190 | 2,090 | 1,870 | 8,350 | 2,630 | 2,500 | 8,110 | 2,870 |
| Minnesota | 29,730 | 3,900 | 130 | 2,140 | 990 | 1,120 | 3,250 | 1,190 | 1,330 | 3,740 | 1,270 |
| Mississippi | 16,260 | 2,050 | 140 | 1,460 | 390 | 450 | 2,340 | 540 | 550 | 2,150 | 500 |
| Missouri | 34,680 | 4,610 | 260 | 2,840 | 1,120 | 1,100 | 5,380 | 1,510 | 1,450 | 3,900 | 1,500 |
| Montana | 5,950 | 830 | † | 500 | 190 | 200 | 760 | 300 | 270 | 1,000 | 310 |
| Nebraska | 9,540 | 1,230 | 60 | 850 | 340 | 320 | 1,200 | 500 | 450 | 1,190 | 440 |
| Nevada | 13,640 | 1,690 | 120 | 1,110 | 350 | 440 | 1,770 | 470 | 530 | 1,640 | 660 |
| New Hampshire | 8,090 | 1,120 | † | 540 | 310 | 260 | 1,140 | 280 | 350 | 1,080 | 450 |
| New Jersey | 51,410 | 7,310 | 410 | 4,260 | 1,850 | 1,610 | 5,830 | 2,520 | 2,310 | 7,270 | 2,530 |
| New Mexico | 9,970 | 1,320 | 80 | 820 | 300 | 360 | 990 | 480 | 410 | 1,290 | 390 |
| New York | 107,840 | 14,900 | 870 | 8,010 | 4,250 | 3,630 | 13,180 | 4,270 | 4,800 | 14,850 | 5,200 |
| North Carolina | 50,420 | 7,820 | 390 | 3,980 | 1,630 | 1,660 | 7,750 | 2,600 | 2,150 | 7,210 | 2,170 |
| North Dakota | 3,840 | 510 | † | 350 | 110 | 140 | 440 | 180 | 170 | 490 | 190 |
| Ohio | 65,010 | 8,950 | 450 | 5,430 | 2,410 | 1,930 | 10,000 | 2,790 | 2,790 | 8,150 | 3,040 |
| Oklahoma | 19,280 | 2,770 | 170 | 1,690 | 540 | 670 | 3,220 | 480 | 840 | 2,480 | 830 |
| Oregon | 22,410 | 3,280 | 130 | 1,510 | 740 | 720 | 2,830 | 1,480 | 960 | 3,110 | 1,090 |
| Pennsylvania | 81,540 | 9,990 | 540 | 6,300 | 3,000 | 2,560 | 10,540 | 3,880 | 3,410 | 10,050 | 4,080 |
| Rhode Island | 6,040 | 730 | † | 470 | 230 | 180 | 880 | 180 | 250 | 760 | 330 |
| South Carolina | 25,550 | 3,820 | 220 | 2,130 | 780 | 820 | 4,040 | 1,420 | 1,070 | 3,870 | 1,090 |
| South Dakota | 4,520 | 600 | † | 360 | 150 | 170 | 570 | 210 | 210 | 550 | 220 |
| Tennessee | 38,300 | 4,770 | 320 | 3,060 | 1,000 | 1,110 | 6,200 | 1,940 | 1,500 | 4,410 | 1,510 |
| Texas | 113,630 | 16,510 | 1,240 | 10,050 | 3,240 | 4,360 | 13,650 | 2,410 | 5,080 | 15,020 | 4,080 |
| Utah | 11,050 | 1,460 | 70 | 670 | 360 | 390 | 660 | 800 | 510 | 1,750 | 430 |
| Vermont | 4,020 | 530 | † | 280 | 150 | 110 | 570 | 150 | 170 | 470 | 210 |
| Virginia | 41,170 | 6,090 | 320 | 2,970 | 1,340 | 1,100 | 5,740 | 2,230 | 1,680 | 6,120 | 1,670 |
| Washington | 38,180 | 5,480 | 230 | 2,700 | 1,250 | 1,300 | 4,790 | 2,460 | 1,770 | 5,430 | 1,790 |
| West Virginia | 11,730 | 1,430 | 90 | 1,080 | 400 | 380 | 2,080 | 550 | 480 | 1,370 | 550 |
| Wisconsin | 32,700 | 4,310 | 190 | 2,460 | 1,160 | 1,190 | 4,370 | 1,330 | 1,460 | 4,310 | 1,610 |
| Wyoming | 2,860 | 390 | † | 230 | 90 | 100 | 320 | 160 | 120 | 460 | 140 |
| United States | 1,658,370 | 231,840 | 12,900 | 132,700 | 54,870 | 54,270 | 221,200 | 73,870 | 71,850 | 220,800 | 74,000 |
*Rounded to the nearest 10; excludes basal cell and squamous cell skin cancers and in situ carcinoma except urinary bladder.
†Estimate is fewer than 50 cases.
Note: These are model-based estimates that should be interpreted with caution. State estimates may not add to US total due to rounding and the exclusionof states with fewer than 50 cases.
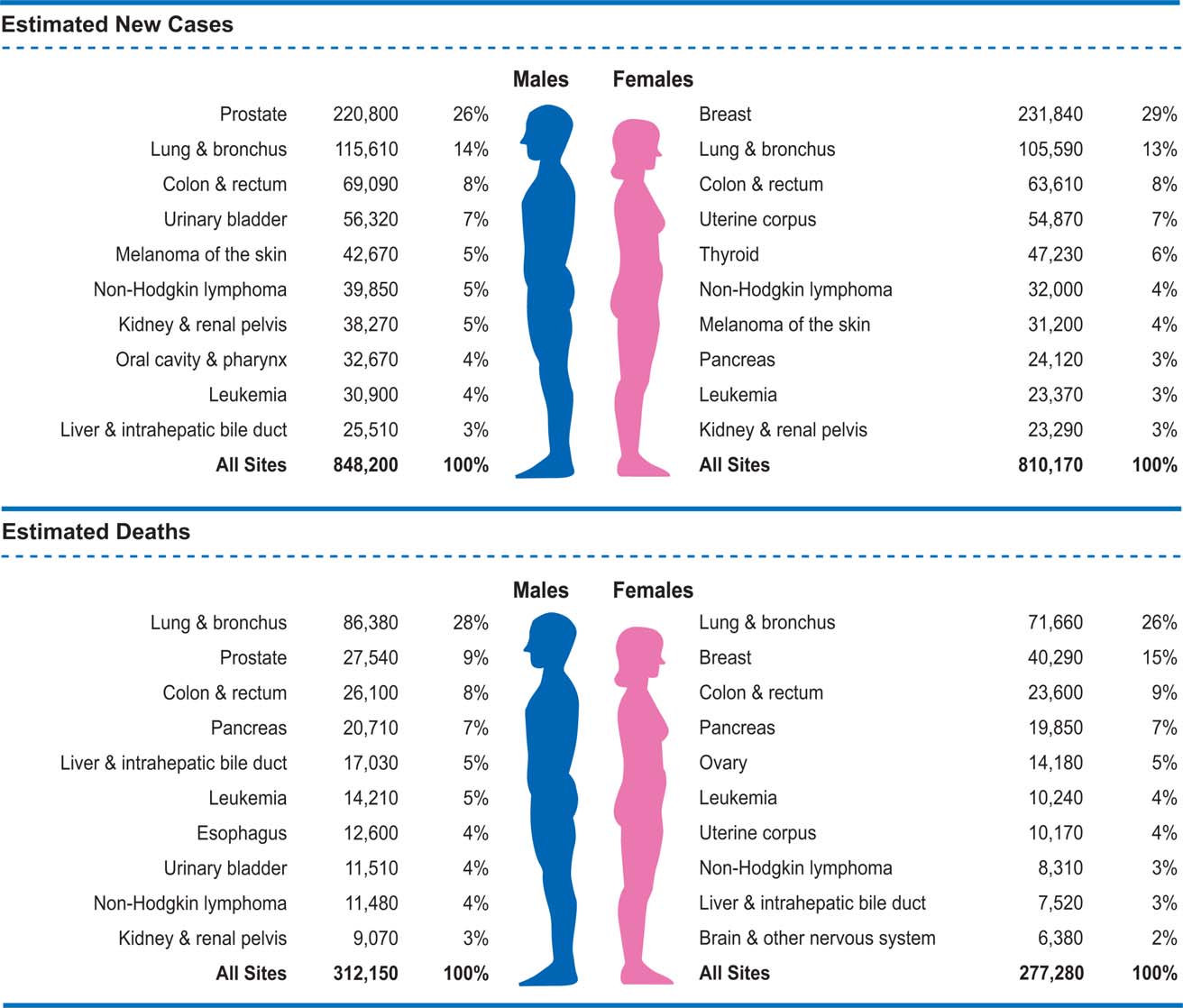
FIGURE 1. Ten Leading Cancer Types for the Estimated New Cancer Cases and Deaths by Sex, United States, 2015.
Estimates are rounded to the nearest 10 and cases exclude basal cell and squamous cell skin cancers and in situ carcinoma except urinary bladder.
As of 1992, SEER data have been available for 4 additional populations (Alaska Natives, Los Angeles county, San Jose-Monterey, and rural Georgia) that increase the coverage of minority groups, allowing for stratification by race and ethnicity.5 Delay-adjusted data from these (SEER 13) registries, which represent 14% of the US population, were the source for the annual percent change in incidence from 1992 to 2011. The SEER program added 5 additional catchment areas beginning with cases diagnosed in 2000 (greater California, greater Georgia, Kentucky, Louisiana, and New Jersey), achieving 28% population coverage. Data from all 18 SEER areas were the source for cancer stage distribution, stage-specific survival, and the lifetime probability of developing cancer.6 Much of the statistical information presented herein was adapted from data previously published in the SEER Cancer Statistics Review, 1975
7
2011.
The North American Association of Central Cancer Registries (NAACCR) compiles and reports incidence data from 1995 onward for cancer registries that participate in the SEER program and/or the NPCR. (Five states receive funding from both programs). These data approach 100% coverage of the US population in the most recent time period and were the source for the projected new cancer cases in 2015, incidence rates by state and race/ethnicity, and the 5-year average annual percent change in incidence rates by race/ethnicity and for childhood and adolescent cancers.8,9 Some of the data presented herein were previously published in volumes 1 and 2 of Cancer in North
10,11
America: 2007-2011.
All cancer cases were classified according to the International Classification of Diseases for Oncology except childhood and adolescent cancers, for which the International Classification of Childhood Cancer (ICCC) was used.12 The lifetime
TABLE 3. Estimated Deaths for Selected Cancers by State, 2015*
| STATE | ALL SITES | BRAIN & OTHER NERVOUS SYSTEM | FEMALE BREAST | COLON & RECTUM | LEUKEMIA | LIVER & INTRAHEPATIC BILE DUCT | LUNG & BRONCHUS | NON-HODGKIN LYMPHOMA | OVARY | PANCREAS | PROSTATE |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Alabama | 10,560 | 290 | 680 | 930 | 420 | 360 | 3,280 | 330 | 270 | 660 | 580 |
| Alaska | 1,040 | † | 70 | 90 | † | 50 | 290 | † | † | 70 | 50 |
| Arizona | 11,540 | 330 | 770 | 990 | 510 | 530 | 2,800 | 410 | 310 | 830 | 600 |
| Arkansas | 6,760 | 160 | 410 | 620 | 260 | 270 | 2,180 | 210 | 140 | 410 | 290 |
| California | 58,180 | 1,690 | 4,320 | 5,180 | 2,550 | 3,250 | 12,370 | 2,070 | 1,530 | 4,240 | 3,180 |
| Colorado | 7,590 | 260 | 540 | 650 | 330 | 350 | 1,710 | 250 | 240 | 530 | 430 |
| Connecticut | 6,840 | 190 | 460 | 440 | 300 | 270 | 1,730 | 220 | 170 | 540 | 360 |
| Delaware | 2,010 | 50 | 120 | 150 | 80 | 90 | 600 | 60 | † | 140 | 100 |
| Dist. of Columbia | 990 | † | 80 | 100 | † | 60 | 210 | † | † | 80 | 70 |
| Florida | 43,050 | 1,000 | 2,830 | 3,520 | 1,790 | 1,710 | 11,920 | 1,440 | 940 | 2,980 | 2,030 |
| Georgia | 16,460 | 430 | 1,240 | 1,500 | 630 | 660 | 4,640 | 470 | 430 | 1,040 | 750 |
| Hawaii | 2,470 | † | 130 | 230 | 100 | 140 | 580 | 90 | 60 | 220 | 110 |
| Idaho | 2,790 | 90 | 190 | 220 | 130 | 90 | 670 | 100 | 60 | 210 | 170 |
| Illinois | 23,940 | 570 | 1,640 | 2,090 | 990 | 860 | 6,550 | 810 | 560 | 1,640 | 1,080 |
| Indiana | 13,420 | 340 | 870 | 1,080 | 570 | 400 | 4,060 | 450 | 300 | 850 | 540 |
| Iowa | 6,440 | 190 | 390 | 570 | 270 | 210 | 1,770 | 250 | 170 | 410 | 300 |
| Kansas | 5,510 | 170 | 350 | 480 | 260 | 190 | 1,540 | 200 | 140 | 380 | 240 |
| Kentucky | 10,200 | 230 | 590 | 850 | 370 | 310 | 3,550 | 320 | 200 | 600 | 350 |
| Louisiana | 9,040 | 210 | 630 | 810 | 330 | 440 | 2,610 | 280 | 180 | 620 | 380 |
| Maine | 3,300 | 90 | 180 | 240 | 140 | 100 | 970 | 110 | 70 | 210 | 150 |
| Maryland | 10,470 | 260 | 810 | 860 | 400 | 440 | 2,700 | 320 | 250 | 780 | 500 |
| Massachusetts | 12,710 | 330 | 770 | 930 | 530 | 580 | 3,420 | 410 | 330 | 930 | 570 |
| Michigan | 20,920 | 580 | 1,410 | 1,670 | 890 | 730 | 6,010 | 740 | 470 | 1,480 | 810 |
| Minnesota | 9,820 | 270 | 620 | 760 | 490 | 370 | 2,450 | 380 | 240 | 660 | 510 |
| Mississippi | 6,360 | 140 | 410 | 640 | 250 | 260 | 1,950 | 170 | 110 | 390 | 300 |
| Missouri | 12,830 | 310 | 900 | 1,050 | 530 | 480 | 3,910 | 400 | 240 | 860 | 500 |
| Montana | 2,020 | 60 | 130 | 170 | 90 | 60 | 540 | 70 | 60 | 140 | 120 |
| Nebraska | 3,480 | 110 | 210 | 340 | 140 | 120 | 890 | 130 | 70 | 240 | 180 |
| Nevada | 4,880 | 150 | 380 | 470 | 190 | 220 | 1,410 | 150 | 110 | 370 | 260 |
| New Hampshire | 2,730 | 80 | 170 | 200 | 110 | 80 | 770 | 80 | 70 | 200 | 120 |
| New Jersey | 16,250 | 380 | 1,290 | 1,480 | 640 | 630 | 3,900 | 510 | 450 | 1,240 | 720 |
| New Mexico | 3,620 | 100 | 270 | 350 | 150 | 180 | 760 | 120 | 110 | 250 | 210 |
| New York | 34,600 | 840 | 2,420 | 2,890 | 1,470 | 1,520 | 8,740 | 1,300 | 900 | 2,590 | 1,640 |
| North Carolina | 19,310 | 460 | 1,340 | 1,490 | 750 | 730 | 5,780 | 590 | 430 | 1,200 | 860 |
| North Dakota | 1,280 | † | 80 | 130 | 60 | † | 320 | † | † | 90 | 70 |
| Ohio | 25,400 | 620 | 1,740 | 2,090 | 1,010 | 850 | 7,370 | 850 | 560 | 1,720 | 1,130 |
| Oklahoma | 8,100 | 220 | 520 | 680 | 320 | 310 | 2,460 | 260 | 180 | 490 | 350 |
| Oregon | 8,040 | 240 | 510 | 670 | 330 | 370 | 2,070 | 280 | 220 | 560 | 420 |
| Pennsylvania | 28,640 | 650 | 1,950 | 2,400 | 1,240 | 1,020 | 7,520 | 1,030 | 700 | 2,050 | 1,280 |
| Rhode Island | 2,120 | 50 | 130 | 160 | 90 | 90 | 570 | 60 | † | 120 | 100 |
| South Carolina | 10,130 | 240 | 690 | 840 | 350 | 380 | 2,970 | 300 | 230 | 640 | 460 |
| South Dakota | 1,630 | 50 | 110 | 140 | 80 | 50 | 450 | 50 | † | 100 | 90 |
| Tennessee | 14,370 | 360 | 890 | 1,220 | 540 | 550 | 4,600 | 450 | 290 | 840 | 580 |
| Texas | 38,520 | 1,010 | 2,710 | 3,470 | 1,620 | 2,260 | 9,580 | 1,260 | 930 | 2,550 | 1,570 |
| Utah | 2,900 | 120 | 270 | 240 | 140 | 120 | 460 | 120 | 90 | 240 | 200 |
| Vermont | 1,360 | † | 80 | 100 | 50 | 60 | 400 | † | † | 90 | 70 |
| Virginia | 14,830 | 370 | 1,090 | 1,180 | 580 | 570 | 4,070 | 480 | 380 | 1,040 | 670 |
| Washington | 12,700 | 400 | 830 | 990 | 540 | 590 | 3,220 | 440 | 350 | 900 | 690 |
| West Virginia | 4,710 | 110 | 270 | 410 | 190 | 130 | 1,460 | 160 | 100 | 250 | 170 |
| Wisconsin | 11,550 | 350 | 720 | 850 | 540 | 400 | 3,050 | 410 | 300 | 830 | 590 |
| Wyoming | 1,000 | † | 70 | 80 | 60 | † | 240 | † | † | 70 | † |
| United States | 589,430 | 15,320 | 40,290 | 49,700 | 24,450 | 24,550 | 158,040 | 19,790 | 14,180 | 40,560 | 27,540 |
*Rounded to the nearest 10.
†Estimate is fewer than 50 deaths.
Note: These are model-based estimates that should be interpreted with caution. State estimates may not add to US total due to rounding and the exclusionof states with fewer than 50 deaths.
TABLE 4. Probability (%) of Developing Invasive Cancer Within Selected Age Intervals by Sex, United States, 2009 to 2011*
| BIRTH TO 49 | 50 TO 59 | 60 TO 69 | �70 | BIRTH TO DEATH | ||
|---|---|---|---|---|---|---|
| All sites† | Male | 3.4 (1 in 29) | 6.7 (1 in 15) | 15.1 (1 in 7) | 36.0 (1 in 3) | 43.3 (1 in 2) |
| Female | 5.4 (1 in 19) | 6.0 (1 in 17) | 10.0 (1 in 10) | 26.4 (1 in 4) | 37.8 (1 in 3) | |
| Breast Colorectum | Female Male | 1.9 (1 in 53) 0.3 (1 in 300) | 2.3 (1 in 44) 0.7 (1 in 148) | 3.5 (1 in 29) 1.3 (1 in 80) | 6.7 (1 in 15) 3.9 (1 in 26) | 12.3 (1 in 8) 4.8 (1 in 21) |
| Female | 0.3 (1 in 326) | 0.5 (1 in 193) | 0.9 (1 in 112) | 3.5 (1 in 28) | 4.5 (1 in 22) | |
| Kidney & renal pelvis | Male Female | 0.2 (1 in 468) 0.1 (1 in 752) | 0.3 (1 in 292) 0.2 (1 in 586) | 0.6 (1 in 157) 0.3 (1 in 321) | 1.3 (1 in 76) 0.7 (1 in 134) | 2.0 (1 in 49) 1.2 (1 in 84) |
| Leukemia | Male | 0.2 (1 in 419) | 0.2 (1 in 598) | 0.4 (1 in 271) | 1.3 (1 in 75) | 1.7 (1 in 59) |
| Lung & bronchus | Female Male | 0.2 (1 in 516) 0.2 (1 in 578) | 0.1 (1 in 968) 0.7 (1 in 140) | 0.2 (1 in 464) 2.0 (1 in 49) | 0.9 (1 in 117) 6.6 (1 in 15) | 1.2 (1 in 84) 7.4 (1 in 13) |
| Female | 0.2 (1 in 541) | 0.6 (1 in 173) | 1.6 (1 in 64) | 4.9 (1 in 20) | 6.2 (1 in 16) | |
| Melanoma of the skin‡ | Male Female | 0.3 (1 in 294) 0.5 (1 in 207) | 0.4 (1 in 240) 0.3 (1 in 323) | 0.8 (1 in 129) 0.4 (1 in 246) | 2.1 (1 in 47) 0.9 (1 in 112) | 3.0 (1 in 34) 1.9 (1 in 53) |
| Non-Hodgkin lymphoma | Male | 0.3 (1 in 366) | 0.3 (1 in 347) | 0.6 (1 in 173) | 1.8 (1 in 55) | 2.4 (1 in 42) |
| Prostate | Female Male | 0.2 (1 in 543) 0.3 (1 in 304) | 0.2 (1 in 483) 2.3 (1 in 44) | 0.4 (1 in 233) 6.3 (1 in 16) | 1.4 (1 in 72) 10.9 (1 in 9) | 1.9 (1 in 52) 15.0 (1 in 7) |
| Thyroid | Male Female | 0.2 (1 in 585) 0.7 (1 in 135) | 0.1 (1 in 827) 0.3 (1 in 288) | 0.2 (1 in 653) 0.3 (1 in 306) | 0.2 (1 in 464) 0.4 (1 in 263) | 0.6 (1 in 174) 1.7 (1 in 60) |
| Uterine cervix | Female | 0.3 (1 in 358) | 0.1 (1 in 840) | 0.1 (1 in 842) | 0.2 (1 in 565) | 0.6 (1 in 154) |
| Uterine corpus | Female | 0.3 (1 in 367) | 0.6 (1 in 170) | 0.9 (1 in 109) | 1.3 (1 in 76) | 2.7 (1 in 37) |
*For people free of cancer at beginning of age interval.
†All sites excludes basal cell and squamous cell skin cancers and in situ cancers except urinary bladder.
‡Probabilities are for whites.
probability of developing cancer was calculated using NCI’s DevCan software (version 6.7.1).13 All incidence and death rates were age-standardized to the 2000 US standard population and expressed per 100,000 population, as calculated by NCI’s SEER*Stat software (version 8.1.5).14 The annual percent change in rates was quantified using NCI’s Joinpoint Regression Program (version 4.1.1).15
Whenever possible, cancer incidence rates presented in this report were adjusted for delays in reporting, which can occur because of a lag in case capture or data corrections. This adjustment is only available for data from the 13 oldest SEER registries because historic patterns of case ascertainment are required to anticipate future corrections to registry data. Delay adjustment has the largest effect on the most recent years of data for cancers that are frequently diagnosed in outpatient settings (eg, melanoma, leukemia, and prostate cancer) and provides a more accurate portrayal of the cancer burden in the most recent time period.16 For example, leukemia incidence rates adjusted for reporting delays are 13% higher than unadjusted rates in the most recent data year.4 Delay-adjusted rates were obtained from SEER*Stat databases.17,18
Projected Cancer Cases and Deaths in 2015
The most recent year for which incidence and mortality data are available lags 3 to 4 years behind the current year due to the time required for data collection, compilation, quality control, and dissemination. Therefore, we project the numbers of new cancer cases and deaths in the United States in the current year in order to provide an estimate of the contemporary cancer burden. These 4-year-ahead projections are not useful for tracking cancer occurrence over time because they are model-based and because the methodology varies over time as we continually strive to achieve the most accurate estimates by taking advantage of improved modeling techniques, increased cancer registration coverage, and updated covariates.
A 3-step spatio-temporal model was used to estimate the number of new invasive cancer cases that will be diagnosed in 2015 based on high-quality incidence data from 49 states (Minnesota data were unavailable) and the District of Columbia during 1995 through 2011. Case coverage represents approximately 89% of the population because, in addition to lacking Minnesota, many states did not achieve high-quality data standards every year. In the first step, complete incidence counts were estimated for each county from 1995 through 2011 using geographic variations in sociodemographic and lifestyle factors, medical settings, and cancer screening behaviors as predictors of incidence.19 Then these counts were adjusted to account for delays in cancer reporting and aggregated to obtain national-and state-level estimates. Finally, a temporal projection method (the vector autoregressive model) was applied to the last 15 years of data to estimate counts for 2015. This method cannot estimate numbers of basal cell or squamous cell skin cancers because data on the occurrence of these cancers are not required to be reported to cancer registries. For the complete details of the case projection methodology, please refer to Zhu et al.20
To estimate the number of cases of female breast carcinoma in situ and melanoma in situ diagnosed in 2015, we first estimated the number of cases occurring annually from 2002 through 2011 by applying age-specific NAACCR incidence rates (data from 44 states with high-quality data every year) to the corresponding US population estimates provided in SEER*Stat.8,14 SEER 13-based delay-adjustment ratios, accessed from NCI’s Cancer Query System,21 were applied to in situ breast cancer counts to account for delays in reporting. (Delay-adjustment ratios are not available for in situ melanoma.) Then the total number of cases in 2015 was projected based on the average annual percent change in case counts from 2002 through 2011 generated by the joinpoint regression model.15
We estimated the number of cancer deaths expected to occur in 2015 in the United States overall and in each state using the joinpoint regression model based on the actual numbers of cancer deaths from 1997 through 2011 at the state and national levels as reported to the NCHS. For the complete details of this methodology, please refer to Chen et al.22
Other Statistics
The estimated number of cancer deaths averted in men and women due to the reduction in overall cancer death rates was calculated by first estimating the number of cancer deaths that would have occurred if death rates had remained at their peak. The expected number of deaths was estimated by applying the 5-year age-specific cancer death rates in the peak year for age-standardized cancer death rates (1990 in men and 1991 in women) to the corresponding age-specific populations in subsequent years through 2011. The difference between the number of expected and recorded cancer deaths in each age group and calendar year was then summed. Averted deaths by state in 2011 were calculated similarly using state-and age-specific average annual crude rates for 5 age groups during 1990 through 1992. An aggregate rate was used instead of a single year because peak years varied across states, with a majority of states reaching peak rates during 1990 to 1992.
Selected Findings
Expected Numbers of New Cancer Cases
Table 1 presents the estimated numbers of new cases of invasive cancer expected in the United States in 2015 by sex. The overall estimate of 1,658,370 new cases is the equivalent of more than 4,500 new cancer diagnoses each day. In addition, about 60,290 cases of female breast carcinoma in situ and 63,440 cases of melanoma in situ are expected to be diagnosed in 2015. The estimated numbers of new cases by state for selected cancer sites are shown in Table 2.
Figure 1 indicates the most common cancers expected to occur in men and women in 2015. Prostate, lung and bronchus, and colorectal cancers will account for about one-half of all cases in men, with prostate cancer alone accounting for about one-quarter of new diagnoses. The 3 most commonly diagnosed cancers in women will be breast, lung and bronchus, and colorectum, accounting for one-half of all cases in women. Breast cancer alone is expected to account for 29% of all new cancers in women.
Expected Numbers of Cancer Deaths
Table 1 also shows the expected numbers of deaths from cancer in 2015. It is estimated that about 589,430 Americans
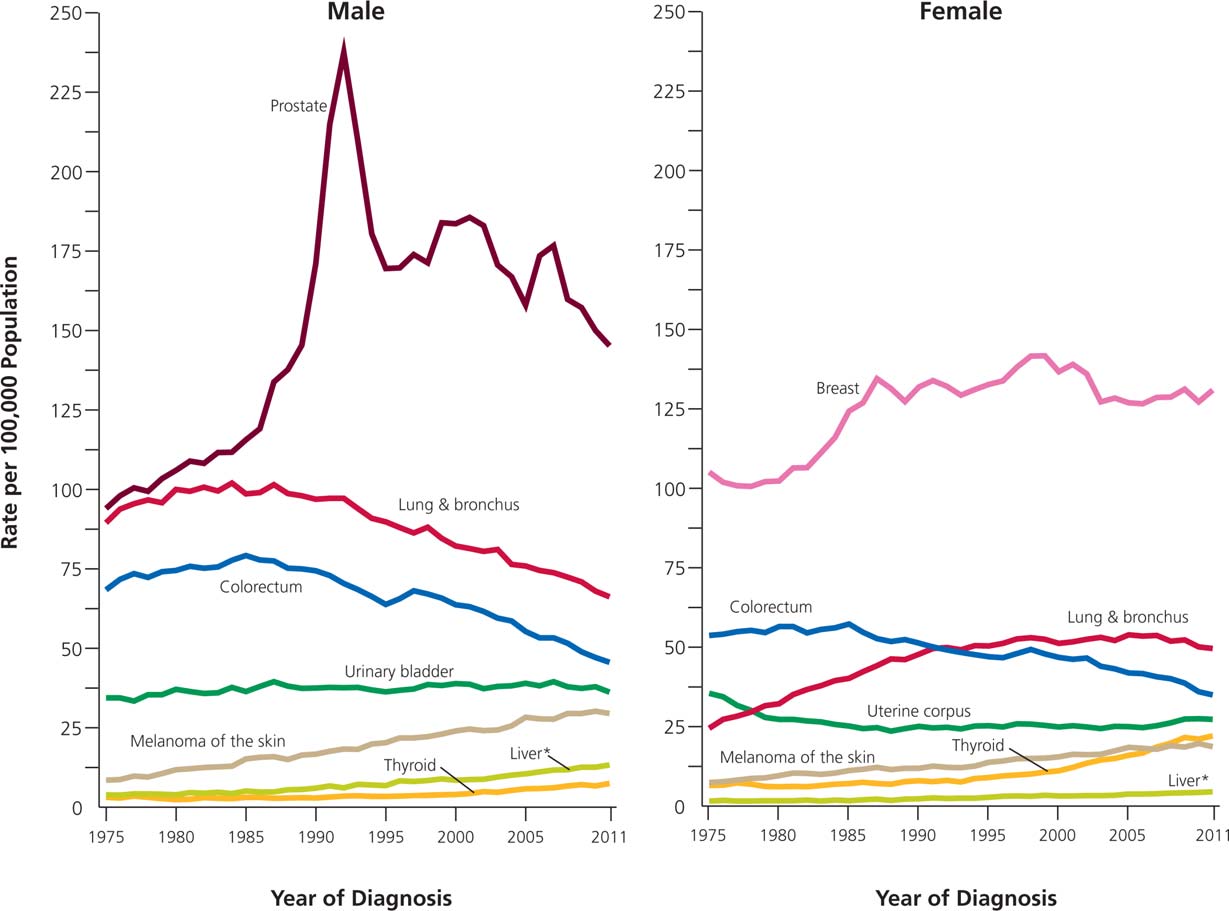
FIGURE 3. Trends in Incidence Rates for Selected Cancers by Sex, United States, 1975 to 2011.
Rates are age adjusted to the 2000 US standard population and adjusted for delays in reporting. *Includes intrahepatic bile duct.
will die from cancer this year, corresponding to about 1,600 deaths per day. The most common causes of cancer death are cancers of the lung and bronchus, prostate, and colorectum in men and cancers of the lung and bronchus, breast, and colorectum in women. These 4 cancers account for almost one-half of all cancer deaths (Fig. 1), with more than one-quarter (27%) of all cancer deaths due to lung cancer. Table 3 provides the estimated numbers of deaths in 2015 by state for selected cancer sites.
Lifetime Probability of Developing Cancer
The lifetime probability of being diagnosed with an invasive cancer is higher for men (43%) than for women (38%) (Table 4). The reasons for increased susceptibility in men are not well understood, but to some extent likely reflect differences in environmental exposures, endogenous hormones, and complex interactions between these influences. Recent studies suggest that height may also be afactor.23,24 For adults aged younger than 50 years, however, cancer risk is higher for women (5.4%) than for men (3.4%) because of the higher occurrence of breast, genital, and thyroid cancers in young women. The current cancer incidence rate among individuals aged birth to 49 years is 78.6 (per 100,000 population) in males and 125.1 in females, compared with 1732.8 and 1188.9, respectively, among adults aged 50 years and older.8 The estimated probability of developing cancer is based on the average experience of the general population and may over-or underestimate individual risk because of differences in exposure (eg, smoking history), medical history, and/or genetic susceptibility.
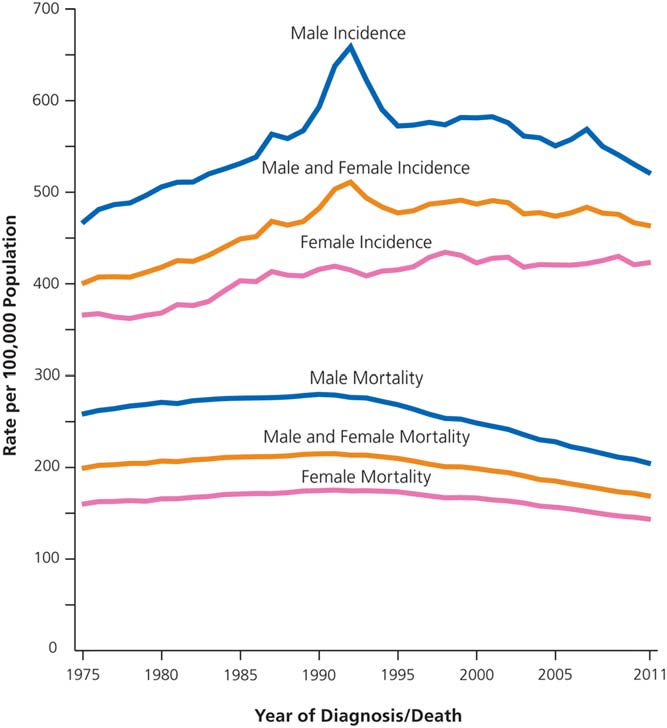
Trends in Cancer Incidence
Figures 2 and 3 illustrate long-term trends in cancer incidence rates for all cancers combined and for selected cancer sites by sex. Cancer incidence patterns in the United States reflect behavioral trends and improvements in cancer prevention and control, as well as changes in medical practice. Trends in overall incidence are heavily influenced by the 4 major cancers (lung, breast, prostate, and colorectal). For example, the steady increase in incidence rates in men from 1975 to the early 1990s (Fig. 2) was driven by a surge in prostate cancer incidence largely due to the increased detection of asymptomatic disease, first through the use of transurethral prostatectomy and then through widespread prostate-specific antigen (PSA) testing (Fig. 3).25,26 The
TABLE 5. Trends in Cancer Incidence (Delay-Adjusted) and Death Rates for Selected Cancers by Sex, United States, 1992 to 2011
| TREND 1 | TREND 2 | TREND 3 | TREND 4 | |||||
| 2007-2011 | ||||||||
| YEARS | APC | YEARS | APC | YEARS | APC | YEARS | APC | AAPC |
| All sites | ||||||||
| Incidence | ||||||||
| Overall 1992-1994 | 23.1 | 1994-1999 | 0.3 | 1999-2011 | 20.5* | 20.5* | ||
| Male 1992-1994 | 25.9* | 1994-2007 | 20.5* | 2007-2011 | 21.8* | 21.8* | ||
| Female 1992-1998 | 0.8* | 1998-2003 | 20.7 | 2003-2011 | 0.0 | 0.0 | ||
| Death | ||||||||
| Overall 1992-2001 | 21.0* | 2001-2011 | 21.5* | 21.5* | ||||
| Male 1992-2001 | 21.4* | 2001-2011 | 21.8* | 21.8* | ||||
| Female 1992-1995 | 20.2 | 1995-1998 | 21.2* | 1998-2001 | 20.4 | 2001-2011 | 21.4* | 21.4* |
| Female breast | ||||||||
| Incidence 1992-1999 | 1.3* | 1999-2004 | 22.2* | 2004-2011 | 0.3 | 0.3 | ||
| Death 1992-1995 | 21.3* | 1995-1998 | 23.4* | 1998-2011 | 21.9* | 21.9* | ||
| Colorectum | ||||||||
| Incidence | ||||||||
| Male 1992-1995 | 22.6* | 1995-1998 | 1.4 | 1998-2008 | 22.5* | 2008-2011 | 24.0* | 23.6* |
| Female 1992-1995 | 21.8* | 1995-1998 | 1.8 | 1998-2008 | 21.9* | 2008-2011 | 24.2* | 23.6* |
| Death | ||||||||
| Male 1992-2002 | 22.0* | 2002-2005 | 23.9* | 2005-2011 | 22.6* | 22.6* | ||
| Female 1992-2001 | 21.7* | 2001-2011 | 23.0* | 23.0* | ||||
| Liver & intrahepatic bile duct | ||||||||
| Incidence | ||||||||
| Male 1992-2011 | 3.6* | 3.6* | ||||||
| Female 1992-2011 | 2.9* | 2.9* | ||||||
| Death | ||||||||
| Male 1992-2007 | 2.2* | 2007-2011 | 3.3* | 3.3* | ||||
| Female 1992-2008 | 1.3* | 2008-2011 | 3.1* | 2.6* | ||||
| Lung & bronchus | ||||||||
| Incidence | ||||||||
| Male 1992-2009 | 21.9* | 2009-2011 | 24.0* | 23.0* | ||||
| Female 1992-2007 | 0.0 | 2007-2011 | 22.2* | 22.2* | ||||
| Death | ||||||||
| Male 1992-2005 | 21.9* | 2005-2011 | 22.9* | 22.9* | ||||
| Female 1992-1995 | 1.4* | 1995-2003 | 0.3* | 2003-2007 | 20.8 | 2007-2011 | 21.9* | 21.9* |
| Melanoma of skin | ||||||||
| Incidence | ||||||||
| Male 1992-2011 | 2.3* | 2.3* | ||||||
| Female 1992-1997 | 4.1* | 1997-2011 | 1.5* | 1.5* | ||||
| Death | ||||||||
| Male 1992-2011 | 0.3* | 0.3* | ||||||
| Female 1992-2011 | 20.5* | 20.5* | ||||||
| Pancreas | ||||||||
| Incidence | ||||||||
| Male 1992-2001 | 0.0 | 2001-2011 | 1.2* | 1.2* | ||||
| Female 1992-1999 | 20.1 | 1999-2011 | 1.1* | 1.1* | ||||
| Death | ||||||||
| Male 1992-1996 | 21.0* | 1996-2011 | 0.3* | 0.3* | ||||
| Female 1992-1997 | 20.4 | 1997-2011 | 0.4* | 0.4* | ||||
| Prostate | ||||||||
| Incidence 1992-1995 | 211.2* | 1995-2000 | 2.3 | 2000-2011 | 22.1* | 22.1* | ||
| Death 1992-1994 | 21.0 | 1994-2004 | 23.8* | 2004-2011 | 23.2* | 23.2* | ||
| Thyroid | ||||||||
| Incidence | ||||||||
| Male 1992-1995 | 23.1 | 1995-2011 | 5.3* | 5.3* | ||||
| Female 1992-1999 | 4.2* | 1999-2009 | 6.9* | 2009-2011 | 2.2 | 4.5* | ||
| Death | ||||||||
| Male 1992-2011 | 1.6* | 1.6* | ||||||
| Female 1992-1994 | 26.0 | 1994-2011 | 0.8* | 0.8* |
APC indicates annual percent change based on incidence (delay-adjusted) and mortality rates age adjusted to the 2000 US standard population; AAPC, average annual percent change.
*The APC or AAPC is significantly different from zero (P < .05).
Note: Trends analyzed by the Joinpoint Regression Program, version 4.1.1, allowing up to 3 joinpoints. Incidence trends based on Surveillance, Epidemiology, and End Results (SEER) 13 areas.
TABLE 6. Trends in 5-Year Relative Survival Rates* (%) by Race and Year of Diagnosis, United States, 1975 to 2010
| 1975 TO | ALL RACES 1987 TO | 2004 TO | 1975 TO | WHITE 1987 TO | 2004 TO | 1975 TO | BLACK 1987 TO | 2004 TO | |
|---|---|---|---|---|---|---|---|---|---|
| 1977 | 1989 | 2010 | 1977 | 1989 | 2010 | 1977 | 1989 | 2010 | |
| All sites | 49 | 55 | 68† | 50 | 57 | 69† | 39 | 43 | 62† |
| Brain & other nervous system | 22 | 29 | 35† | 22 | 28 | 33† | 25 | 32 | 42† |
| Breast (female) | 75 | 84 | 91† | 76 | 85 | 92† | 62 | 71 | 80† |
| Colon | 51 | 60 | 65† | 51 | 61 | 67† | 45 | 52 | 56† |
| Esophagus | 5 | 9 | 20† | 6 | 11 | 21† | 4 | 7 | 13† |
| Hodgkin lymphoma | 72 | 79 | 88† | 72 | 80 | 88† | 70 | 72 | 85† |
| Kidney & renal pelvis | 50 | 57 | 74† | 50 | 57 | 74† | 49 | 55 | 72† |
| Larynx | 66 | 66 | 63† | 67 | 67 | 64 | 58 | 56 | 52 |
| Leukemia | 34 | 43 | 60† | 35 | 44 | 61† | 33 | 35 | 54† |
| Liver & intrahepatic bile duct | 3 | 5 | 18† | 3 | 6 | 17† | 2 | 3 | 13† |
| Lung & bronchus | 12 | 13 | 18† | 12 | 13 | 18† | 11 | 11 | 15† |
| Melanoma of the skin | 82 | 88 | 93† | 82 | 88 | 93† | 57‡ | 79‡ | 75 |
| Myeloma | 25 | 27 | 47† | 24 | 27 | 47† | 30 | 30 | 47† |
| Non-Hodgkin lymphoma | 47 | 51 | 71† | 47 | 51 | 73† | 48 | 46 | 63† |
| Oral cavity & pharynx | 53 | 54 | 66† | 54 | 56 | 67† | 36 | 34 | 45† |
| Ovary | 36 | 38 | 45† | 35 | 38 | 44† | 42 | 34 | 36 |
| Pancreas | 3 | 4 | 7† | 3 | 3 | 7† | 2 | 6 | 7† |
| Prostate | 68 | 83 | >99† | 69 | 84 | >99† | 61 | 71 | 98† |
| Rectum | 48 | 58 | 68† | 48 | 59 | 68† | 44 | 52 | 63† |
| Stomach | 15 | 20 | 29† | 14 | 18 | 28† | 16 | 19 | 28† |
| Testis | 83 | 95 | 97† | 83 | 96 | 97† | 73‡§ | 88‡ | 90 |
| Thyroid | 92 | 94 | 98† | 92 | 94 | 98† | 90 | 92 | 96† |
| Urinary bladder | 72 | 79 | 79† | 73 | 80 | 80† | 50 | 63 | 64† |
| Uterine cervix | 69 | 70 | 70 | 70 | 73 | 71 | 65 | 57 | 62 |
| Uterine corpus | 87 | 82 | 83† | 88 | 84 | 85† | 60 | 57 | 65† |
*Survival rates are adjusted for normal life expectancy and are based on cases diagnosed in the Surveillance, Epidemiology, and End Results (SEER) 9 areas from 1975 to 1977, 1987 to 1989, and 2004 to 2010, all followed through 2011.
†The difference in rates between 1975 to 1977 and 2004 to 2010 is statistically significant (P <.05).
‡The standard error of the survival rate is between 5 and 10 percentage points. §Survival rate is for 1978 to 1980.
increase in incidence in women during the 1980s reflects the increase in lung cancer as a result of the tobacco epidemic and the increase in breast cancer because of changes in female reproductive patterns, as well as increased detection of asymptomatic disease during the rapid uptake of mammography screening.27
Table 5 presents the annual percent change in delay-adjusted incidence rates in the SEER 13 registries during 1992 through 2011 based on joinpoint regression analysis. Joinpoint is a tool used to describe and quantify trends by fitting observed rates to lines connected at “joinpoints” where trends change in direction or magnitude.7,28 During the past 5 years for which there are data (2007-2011), the overall incidence rate remained stable in women and declined by 1.8% per year in men. The decrease in men is driven by the rapid declines in colorectal (3.6% per year), lung (3.0% per year), and prostate (2.1% per year) cancers. Among women, although the recent rates of decline for colorectal and lung cancers have been similar to those in men, breast cancer incidence rates remained flat and thyroid cancer incidence rates increased dramatically, by an average of 4.5% per year from 2007 to 2011. Although thyroid cancer incidence is also increasing rapidly in men, the 3-fold higher rates in women have a larger influence on overall trends.8
The long-term declines in colorectal cancer incidence rates since the mid-1980s have been attributed to both changes in risk factors and the introduction of colorectal cancer screening.29 However, the rapid declines in recent years (4.0% or greater per year from 2008-2011) likely reflect the increased uptake of screening, primarily in the form of colonoscopy, which can prevent cancer by allowing for the removal of precancerous lesions.30,31 Among adults aged 50 to 75 years, colonoscopy use increased from 19.1% in 2000 to 54.5% in 2013.32
Lung cancer incidence rates began declining in the mid-1980s in men and in the late 1990s in women as a result of reductions in smoking prevalence that began decades earlier. Contemporary differences in lung cancer incidence patterns between men and women (Fig. 3) reflect historical differences in tobacco use. Women took up smoking in large numbers decades later than men, first
TABLE 7. Relative Decline in Cancer Death Rates by State Since the Early 1990s and Potential Deaths Averted in 2011
| 1990 TO | 2011 | RELATIVE | 2011 OBSERVED | 2011 EXPECTED | 2011 AVERTED | |
|---|---|---|---|---|---|---|
| 1992 RATE | RATE | DECLINE | COUNTS* | COUNTS† | DEATHS‡ | |
| Alabama | 220.2 | 187.4 | 15% | 10,233 | 12,122 | 1,889 |
| Alaska | 219.3 | 176.1 | 20% | 935 | 1,204 | 269 |
| Arizona | 197.8 | 148.4 | 25% | 10,690 | 14,363 | 3,673 |
| Arkansas | 221.8 | 191.1 | 14% | 6,497 | 7,625 | 1,128 |
| California | 202.2 | 151.8 | 25% | 56,448 | 76,129 | 19,681 |
| Colorado | 187.5 | 143.9 | 23% | 7,051 | 9,416 | 2,365 |
| Connecticut | 206.9 | 157.9 | 24% | 6,837 | 8,948 | 2,111 |
| Delaware | 240.9 | 179.7 | 25% | 1,905 | 2,583 | 678 |
| Dist. of Columbia | 269.7 | 180.6 | 33% | 1,070 | 1,629 | 559 |
| Florida | 208.0 | 160.2 | 23% | 41,681 | 53,723 | 12,042 |
| Georgia | 214.8 | 171.0 | 20% | 15,602 | 20,184 | 4,582 |
| Hawaii | 172.5 | 138.2 | 20% | 2,278 | 2,841 | 563 |
| Idaho | 187.0 | 157.6 | 16% | 2,573 | 3,111 | 538 |
| Illinois | 222.9 | 174.8 | 22% | 24,006 | 31,036 | 7,030 |
| Indiana | 221.0 | 185.2 | 16% | 13,180 | 15,966 | 2,786 |
| Iowa | 198.5 | 172.4 | 13% | 6,481 | 7,502 | 1,021 |
| Kansas | 197.2 | 169.9 | 14% | 5,440 | 6,343 | 903 |
| Kentucky | 236.3 | 200.9 | 15% | 9,733 | 11,726 | 1,993 |
| Louisiana | 240.4 | 193.5 | 20% | 9,233 | 11,646 | 2,413 |
| Maine | 230.5 | 181.7 | 21% | 3,201 | 4,087 | 886 |
| Maryland | 237.3 | 165.9 | 30% | 10,249 | 14,865 | 4,616 |
| Massachusetts | 225.1 | 166.4 | 26% | 12,895 | 17,531 | 4,636 |
| Michigan | 220.2 | 177.4 | 19% | 20,420 | 25,597 | 5,177 |
| Minnesota | 197.8 | 160.5 | 19% | 9,489 | 11,849 | 2,360 |
| Mississippi | 224.2 | 196.8 | 12% | 6,278 | 7,233 | 955 |
| Missouri | 217.5 | 179.4 | 18% | 12,473 | 15,311 | 2,838 |
| Montana | 203.4 | 164.4 | 19% | 2,022 | 2,547 | 525 |
| Nebraska | 192.9 | 164.2 | 15% | 3,410 | 4,052 | 642 |
| Nevada | 226.7 | 170.3 | 25% | 4,605 | 6,308 | 1,703 |
| New Hampshire | 224.0 | 178.0 | 21% | 2,740 | 3,510 | 770 |
| New Jersey | 229.6 | 165.6 | 28% | 16,708 | 23,332 | 6,624 |
| New Mexico | 182.5 | 146.6 | 20% | 3,328 | 4,200 | 872 |
| New York | 215.4 | 159.6 | 26% | 35,469 | 47,934 | 12,465 |
| North Carolina | 213.9 | 174.8 | 18% | 18,284 | 22,694 | 4,410 |
| North Dakota | 199.1 | 160.5 | 19% | 1,321 | 1,644 | 323 |
| Ohio | 224.2 | 184.4 | 18% | 25,140 | 30,880 | 5,740 |
| Oklahoma | 209.6 | 191.2 | 9% | 7,997 | 8,859 | 862 |
| Oregon | 209.2 | 172.2 | 18% | 7,802 | 9,668 | 1,866 |
| Pennsylvania | 223.6 | 177.3 | 21% | 28,895 | 36,398 | 7,503 |
| Rhode Island | 222.7 | 168.3 | 24% | 2,170 | 2,888 | 718 |
| South Carolina | 219.7 | 182.2 | 17% | 9,543 | 11,662 | 2,119 |
| South Dakota | 195.9 | 168.6 | 14% | 1,665 | 1,930 | 265 |
| Tennessee | 220.6 | 189.1 | 14% | 13,562 | 16,015 | 2,453 |
| Texas | 211.3 | 162.6 | 23% | 37,351 | 49,696 | 12,345 |
| Utah | 157.4 | 125.6 | 20% | 2,746 | 3,469 | 723 |
| Vermont | 218.9 | 175.6 | 20% | 1,347 | 1,735 | 388 |
| Virginia | 222.1 | 170.7 | 23% | 14,374 | 19,125 | 4,751 |
| Washington | 205.9 | 166.6 | 19% | 12,002 | 15,194 | 3,192 |
| West Virginia | 226.8 | 199.6 | 12% | 4,782 | 5,569 | 787 |
| Wisconsin | 208.1 | 174.9 | 16% | 11,608 | 13,950 | 2,342 |
| Wyoming | 193.2 | 156.1 | 19% | 936 | 1,192 | 256 |
Rates are per 100,000 and age adjusted to the 2000 US standard population. *Excludes unknown age.
†Expected counts were estimated by applying age-specific crude rates for 1990–1992 to 2011 population estimates.
‡Deaths averted is the difference between the number of expected and observed deaths in 2011.
initiated smoking at older ages, and were slower to quit, The decline in prostate cancer incidence rates that including recent upturns in smoking prevalence in some began in the mid-1990s likely reflects the diminishing birth cohorts.33,34 proportion of men receiving an initial PSA test.35
TABLE 8. Ten Leading Causes of Death by Age and Sex, United States, 2011
| ALL AGES MALE FEMALE All Causes All Causes 1,254,978 1,260,480 | AGES 1 TO 19 MALE FEMALE All Causes All Causes 13,202 7,039 | AGES 20 TO 39 MALE FEMALE All Causes All Causes 61,744 28,555 | AGES 40 TO 59 MALE FEMALE All Causes All Causes 226,700 143,234 | AGES 60 TO 79 MALE FEMALE All Causes All Causes 484,159 382,212 | AGES �80 MALE FEMALE All Causes All Causes 455,747 688,747 | |
|---|---|---|---|---|---|---|
| 1 | Heart diseases 308,398 Heart diseases 288,179 | Accidents (unintentional injuries) 4,916 Accidents (unintentional injuries) 2,394 | Accidents (unintentional injuries) 22,459 Accidents (unintentional injuries) 8,122 | Cancer 54,172 Cancer 50,445 | Cancer 158,118 Cancer 129,632 | Heart diseases 132,189 Heart diseases 191,463 |
| 2 | Cancer 302,231 Cancer 274,460 | Assault (homicide) 1,862 Cancer 797 | Intentional self-harm (suicide) 9,708 Cancer 4,407 | Heart diseases 52,247 Heart diseases 21,470 | Heart diseases 118,232 Heart diseases 72,365 | Cancer 84,860 Cancer 89,145 |
| 3 | Accidents (unintentional injuries) 79,257 Cerebrovascular disease 76,597 | Intentional self-harm (suicide) 1,633 Assault (homicide) 513 | Assault (homicide) 7,051 Heart diseases 2,446 | Accidents (unintentional injuries) 25,372 Accidents (unintentional injuries) 12,132 | Chronic lower respiratory diseases 32,493 Chronic lower respiratory diseases 31,990 | Chronic lower respiratory diseases 29,122 Alzheimer disease 51,567 |
| 4 | Chronic lower respiratory diseases 67,521 Chronic lower respiratory diseases 75,422 | Cancer 1,055 Congenital anomalies 464 | Heart diseases 5,143 Intentional self-harm (suicide) 2,409 | Intentional self-harm (suicide) 12,287 Chronic lower respiratory diseases 5,428 | Cerebrovascular disease 19,925 Cerebrovascular disease 19,350 | Cerebrovascular disease 25,029 Cerebrovascular disease 51,528 |
| 5 | Cerebrovascular disease 52,335 Alzheimer disease 59,297 | Congenital anomalies 594 Intentional self-harm (suicide) 456 | Cancer 3,984 Assault (homicide) 1,359 | Chronic liver disease & cirrhosis 11,123 Chronic liver disease & cirrhosis 5,298 | Diabetes mellitus 18,200 Diabetes mellitus 14,392 | Alzheimer disease 20,171 Chronic lower respiratory diseases 37,645 |
| 6 | Diabetes mellitus 38,324 Accidents (unintentional injuries) 47,181 | Heart diseases 403 Heart diseases 283 | HIV disease 879 Pregnancy, childbirth & puerperium 684 | Diabetes mellitus 7,795 Cerebrovascular disease 4,994 | Accidents (unintentional injuries) 14,138 Accidents (unintentional injuries) 8,345 | Influenza & pneumonia 14,189 Influenza & pneumonia 19,413 |
| 7 | Intentional self-harm (suicide) 31,003 Diabetes mellitus 35,507 | Chronic lower respiratory diseases 172 Influenza & pneumonia 138 | Diabetes mellitus 842 Diabetes mellitus 593 | Cerebrovascular disease 6,557 Diabetes mellitus 4,867 | Nephritis, nephrotic syndrome & nephrosis 8,596 Nephritis, nephrotic syndrome & nephrosis 7,589 | Accidents (unintentional injuries) 11,706 Accidents (unintentional injuries) 15,671 |
| 8 | Alzheimer disease 25,677 Influenza & pneumonia 28,425 | Influenza & pneumonia 158 Chronic lower respiratory diseases 86 | Chronic liver disease & cirrhosis 821 Cerebrovascular disease 581 | Chronic lower respiratory diseases 5,393 Intentional self-harm (suicide) 3,981 | Chronic liver disease & cirrhosis 8,264 Alzheimer disease 7,530 | Diabetes mellitus 11,443 Diabetes mellitus 15,616 |
| 9 | Influenza & pneumonia 25,401 Nephritis, nephrotic syndrome & nephrosis 22,942 | Cerebrovascular disease 114 Septicemia 86 | Cerebrovascular disease 634 HIV disease 522 | HIV disease 3,567 Septicemia 2,409 | Influenza & pneumonia 7,741 Septicemia 6,897 | Nephritis, nephrotic syndrome & nephrosis 11,184 Nephritis, nephrotic syndrome & nephrosis 13,284 |
| 10 | Nephritis, nephritic syndrome & nephrosis 22,649 Septicemia 19,264 | Septicemia 86 Cerebrovascular disease 84 | Influenza & pneumonia 556 Chronic liver disease & cirrhosis 471 | Viral hepatitis 3,347 Influenza & pneumonia 1,947 | Septicemia 7,001 Influenza & pneumonia 6,408 | Parkinson disease 8,744 Hypertension & hypertensive renal disease* 11,615 |
HIV indicates human immunodeficiency virus. *Includes primary and secondary hypertension. Note: Deaths within each age group do not sum to all ages combined due to the inclusion of unknown ages. In accordance with the National Center for Health Statistics’
cause-of-death ranking, "Symptoms, signs, and abnormal clinical or laboratory findings" and categories that begin with “Other” and “All other” were not ranked. Source: US Final Mortality Data, 2011, National Center for Health Statistics, Centers for Disease Control and Prevention, 2014.
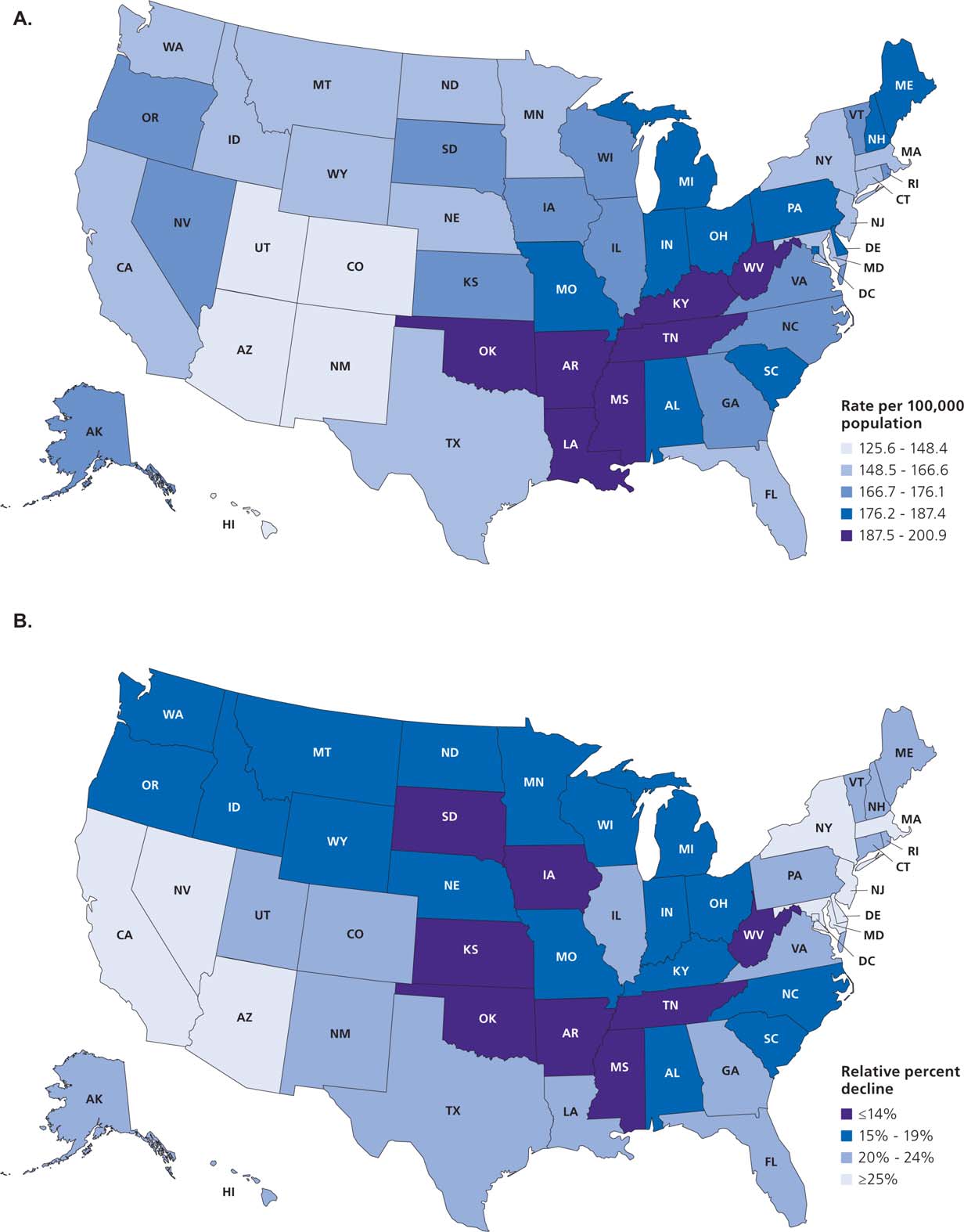
FIGURE 4. Geographic Patterns in Cancer Death Rates in 2011 (A) and in the Relative Decline (%) in Cancer Death Rates from 1990–1992 to 2011 (B).
Rates are per 100,000 and age adjusted to the 2000 US standard population.
Routine screening with the PSA test is no longer rec-declined in recent years among men aged younger than ommended because of growing concerns about high 50 years, as well as in those aged 75 years or older, rates of overdiagnosis, estimated at 23% to 42% for but remain high for older men with a limited life
36 37–39
screen-detected cancers. PSA testing rates may have expectancy.
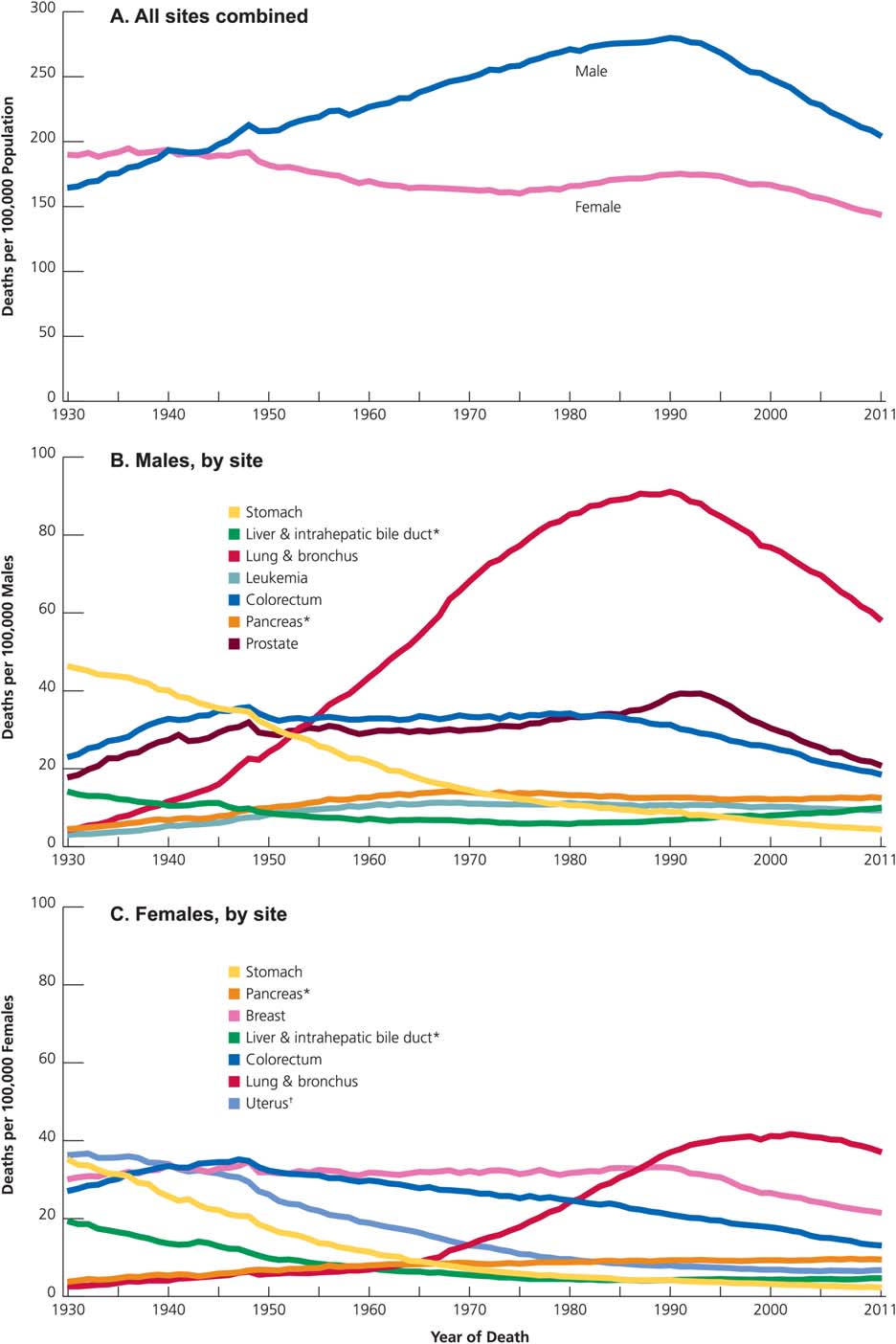
FIGURE 5. Trends in Death Rates Overall and for Selected Sites by Sex, United States, 1930 to 2011.
Rates are age adjusted to the 2000 US standard population. Due to changes in International Classification of Diseases (ICD) coding, numerator information has changed over time. Rates for cancers of the lung and bronchus, colorectum, liver, uterus, and ovary are affected by these changes. *Mortality rates for pancreatic and liver cancers are increasing.
† Uterus includes uterine cervix and uterine corpus.
In contrast to the stable or declining trends for most cancers, incidence rates in the SEER 13 registries increased from 2007 through 2011 among both men and women for cancers of the small intestine, anus, liver, pancreas, soft tissue (including the heart), and thyroid; melanoma of the skin; myeloma; and leuke
mia.7,17
In addition, incidence rates increased in men for breast cancer, non-Hodgkin lymphoma, and human papillomavirus-positive oropharyngeal cancers and in women for esophageal adenocarcinoma and uterine cancer. The largest annual increases were for cancers of the thyroid (5.3% and 4.5% in men and women, respectively) and liver (3.6% and 2.9% in men and women, respectively) (Table 5).
TABLE 9. Five Leading Types of Cancer Death by Age and Sex, United States, 2011
| ALL AGES | <20 | 20 TO 39 | 40 TO 59 | 60 TO 79 | �80 |
| MALE | |||||
| ALL SITES 302,231 Lung & bronchus 86,738 Prostate 27,970 Colorectum 26,804 Pancreas 18,881 Liver* 14,626 | ALL SITES 1,094 Brain & ONS 308 Leukemia 293 Bones & joints 107 Soft tissue (including heart) 80 NHL 44 | ALL SITES 3,984 Leukemia 529 Brain & ONS 491 Colorectum 442 NHL 278 Soft tissue (including heart) 225 | ALL SITES 54,172 Lung & bronchus 14,347 Colorectum 5,789 Liver* 4,754 Pancreas 3,676 Esophagus 2,691 | ALL SITES 158,118 Lung & bronchus 51,951 Colorectum 13,088 Prostate 11,732 Pancreas 10,594 Liver* 7,467 | ALL SITES 84,860 Lung & bronchus 20,216 Prostate 14,956 Colorectum 7,480 Urinary bladder 4,785 Pancreas 4,510 |
| FEMALE | |||||
| ALL SITES 274,460 Lung & bronchus 70,219 Breast 40,931 Colorectum 24,979 Pancreas 18,463 Ovary 14,346 | ALL SITES 828 Brain & ONS 242 Leukemia 226 Soft tissue (including heart) 68 Bones & joints 67 Kidney & renal pelvis 23 | ALL SITES 4,407 Breast 1,041 Uterine cervix 417 Leukemia 356 Colorectum 344 Brain & ONS 303 | ALL SITES 50,445 Breast 11,340 Lung & bronchus 11,043 Colorectum 4,209 Ovary 3,064 Pancreas 2,578 | ALL SITES 129,632 Lung & bronchus 39,287 Breast 17,538 Colorectum 10,084 Pancreas 9,076 Ovary 7,192 | ALL SITES 89,145 Lung & bronchus 19,694 Breast 11,010 Colorectum 10,338 Pancreas 6,747 Leukemia 4,111 |
NHL indicates Non-Hodgkin lymphoma; ONS, other nervous system. *Liver includes intrahepatic bile duct. Note: Ranking order excludes category titles that begin with “Other.”
Trends in Cancer Survival
There have been notable improvements in survival over the past 3 decades for most cancer types in both blacks and whites (Table 6). The 5-year relative survival rate for all sites combined has increased 19 percentage points among whites and 23 percentage points among blacks. Progress has been most rapid for hematopoietic and lymphoid malignancies due to improvements in treatment protocols, including the discovery of targeted therapies. For example, the 5-year survival for acute lymphocytic leukemia increased from 41% during the mid-1970s to 70% during 2004 to 2010. The use of BCR-ABL tyrosine kinase inhibitors (eg, imatinib) doubled survival for patients with chronic myeloid leukemia in less than 2 decades, from 31% in the early 1990s to 60% in 2004 through 2010.40
In contrast to the steady increase in survival for most cancers, advances have been slow for lung and pancreatic cancers, for which the 5-year relative survival is currently 18% and 7%, respectively. These low rates are partly because more than one-half of cases are diagnosed at a distant stage, for which 5-year survival is 4% and 2%, respectively. There is promise for improving lung cancer survival rates because of earlier detection through screening with spiral computed tomography, which has been shown to reduce lung cancer deaths by 16% to 20% among adults with at least a 30-packyear smoking history.41,42 However, it is important to realize that screening, as well as other changes in detection practices, introduces lead time bias in survival rates, thereby reducing their usefulness in measuring progress against cancer. 43 Advances against cancer are best measured using age-standardized mortality rates.
Trends in Cancer Mortality
The overall cancer death rate rose during most of the 20th century, peaking in 1991. This increase was largely driven by rapid increases in lung cancer deaths among men as a consequence of the tobacco epidemic. Over the past 2 decades, however, there has been a steady decline in the cancer death
| NON-HISPANIC WHITE | NON-HISPANIC BLACK | ASIAN/PACIFIC ISLANDER | AMERICAN INDIAN/ ALASKA NATIVE* | HISPANIC | |
|---|---|---|---|---|---|
| Incidence | |||||
| All sites Male Female Breast (female) Colorectum Male Female Kidney & renal pelvis Male Female Liver & intrahepatic bile duct Male Female Lung & bronchus Male Female Prostate Stomach Male Female Uterine cervix | 540.8 435.8 127.6 49.2 37.4 21.6 11.3 8.9 3.0 81.3 59.3 133.2 7.8 3.5 7.1 | 606.2 406.3 123.0 61.9 45.6 24.1 12.9 16.0 4.6 95.4 51.7 219.8 15.4 8.1 10.2 | 322.3 283.7 86.0 39.9 30.0 10.7 5.0 21.2 8.0 48.0 28.0 72.5 15.3 8.6 6.4 | 432.2 368.3 91.7 50.9 41.1 30.1 17.8 18.4 8.6 68.5 52.5 97.9 12.0 6.5 9.5 | 420.9 330.1 91.6 45.9 31.6 20.6 11.6 19.1 6.9 45.0 26.3 120.2 13.8 7.9 10.5 |
| Mortality | |||||
| All sites Male Female Breast (female) Colorectum Male Female Kidney & renal pelvis Male Female Liver & intrahepatic bile duct Male Female Lung & bronchus Male Female Prostate Stomach Male Female Uterine cervix | 214.0 151.2 22.2 18.7 13.2 5.9 2.6 7.3 3.0 63.9 42.1 20.7 3.8 1.9 2.0 | 275.5 173.0 31.4 28.4 18.9 5.8 2.7 12.4 4.3 77.5 37.4 49.8 9.8 4.6 4.2 | 131.0 91.5 11.3 13.1 9.5 3.0 1.3 14.5 6.0 34.7 18.4 10.0 8.3 4.8 1.8 | 190.0 135.2 15.2 19.2 15.6 9.5 4.4 13.8 6.0 50.0 32.4 21.2 7.0 3.8 3.4 | 150.1 99.9 14.5 15.8 9.9 5.1 2.3 12.6 5.5 30.5 14.0 18.5 7.5 4.2 2.8 |
Rates are per 100,000 population and age adjusted to the 2000 US standard population. Nonwhite and nonblack race categories are not mutually exclusive of Hispanic origin.
*Data based on Indian Health Service Contract Health Service Delivery Areas (CHSDA) counties. Incidence rates exclude data from Kansas.
rate as a result of fewer Americans smoking and advances in cancer prevention, early detection, and treatment. The 22% drop in cancer death rates from 1991 (215.1 per 100,000 population) to 2011 (168.7 per 100,000 population) translates into the avoidance of an estimated 1,519,300 cancer deaths (1,071,600 in men and 447,700 in women) that would have occurred if peak rates had persisted.
Although cancer death rates have declined in every state, there is much variation in the magnitude of the declines. Table 7 shows the relative decline in cancer death rates by state from the early 1990s to 2011 and the estimated number of cancer deaths averted in 2011 as a result. The decline was calculated from an average annual baseline rate during 1990 to 1992 because the death rate did not peak in 1991 in all states. Declines ranged from 9% in Oklahoma to 33% in the District of Columbia, and were generally largest in northeastern states. The declines of 25% to 30% in Maryland,
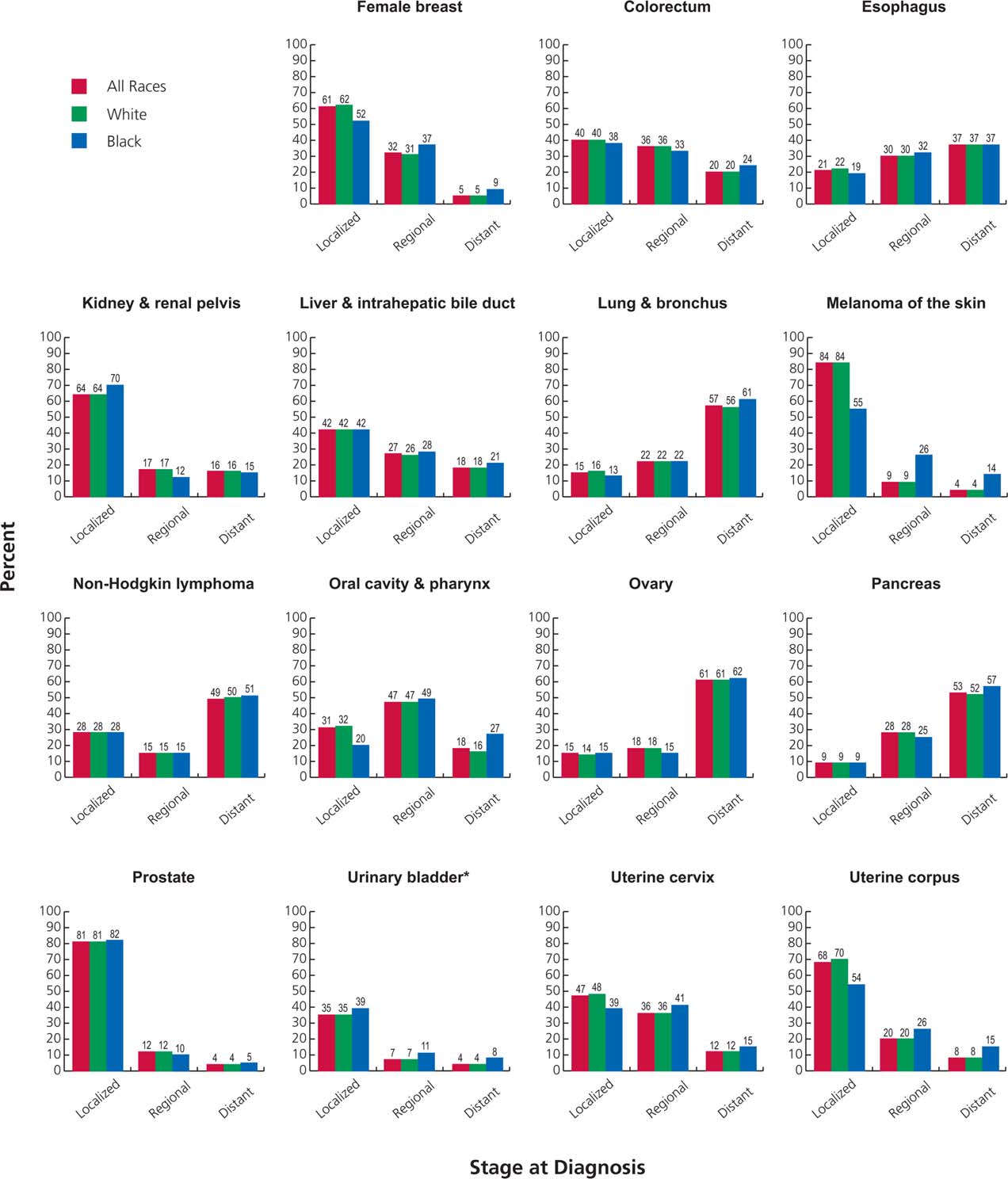
FIGURE 6. Stage Distribution of Selected Cancers by Race, United States, 2004 to 2010.
Stage categories do not sum to 100% because sufficient information is not available to stage all cases. *The proportion of cases of carcinoma in situ of the urinary bladder is 51% in all races combined, 52% in whites, and 39% in blacks.
New Jersey, Massachusetts, New York, and Delaware resulted in 29,000 fewer cancer deaths, collectively, in 2011. Almost 20,000 deaths were averted in California because of a 25% drop. In general, Southern states had the slowest declines and the highest current death rates, whereas western states had the lowest death rates (Fig. 4). For example, 2011 cancer death rates ranged from 125.6 (per 100,000 population) in Utah to 200.9 in Kentucky. The large geographic variation in cancer death rates and trends reflects differences in risk factor patterns, such as smoking and obesity, as well as disparities in the national distribution of poverty and access to health care, which have increased over
time.44,45
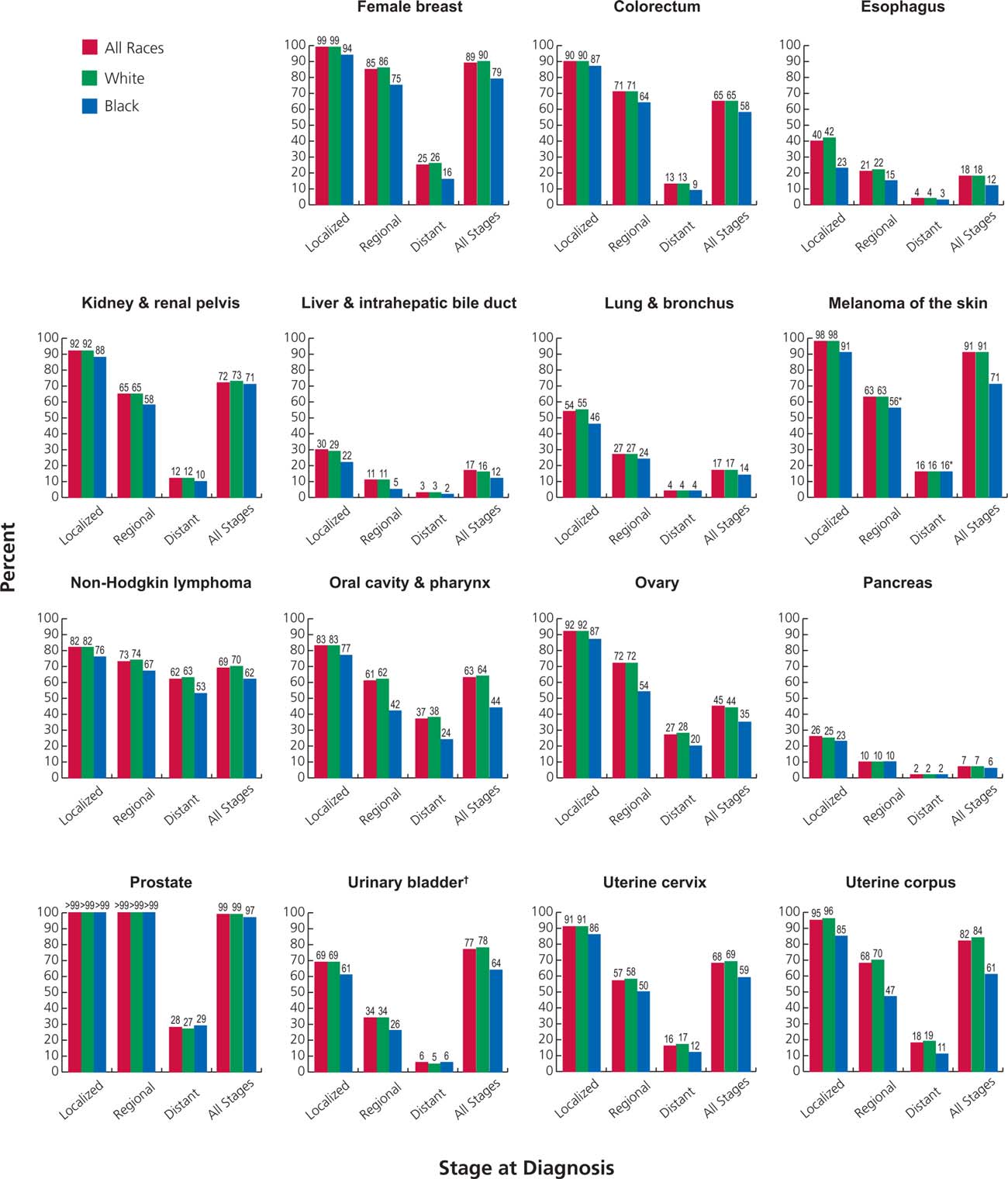
FIGURE 7. Five-Year Relative Survival Rates for Selected Cancers by Race and Stage at Diagnosis, United States, 2004 to 2010.
*The standard error of the survival rate is between 5 and 10 percentage points.
†
The survival rate for carcinoma in situ of the urinary bladder is 96% in all races combined, 96% in whites, and 90% in blacks.
| Figure 5 depicts trends in cancer death rates since 1930 among men and women overall and for selected cancer sites by sex. In contrast to male cancer death rates, which rose continuously prior to 1990, female cancer death rates fell from the late 1940s to the mid-1970s (Fig. 5A). It is also interesting to note that prior to 1941, death rates were | higher in women than in men due to the high death rate for uterine cancer (uterine corpus and uterine cervix combined), which was the leading cause of cancer death among women in the early 20th century. Uterine cancer death rates declined by more than 80% between 1930 and 2011, largely due to the widespread uptake of screening | |
|---|---|---|
| 18 | CA: A Cancer Journal for Clinicians | |
| MALE | INCIDENCE | FEMALE | 5-YEAR AAPC | MALE | MORTALITY | FEMALE | |
|---|---|---|---|---|---|---|---|
| Non-Hispanic white | 22.9* | 20.8 | 21.6* | 21.3* | |||
| Non-Hispanic black | 23.0* | 20.4* | 22.5* | 21.1* | |||
| Asian/Pacific Islander | 21.6* | 0.1 | 21.3* | 20.8* | |||
| American Indian/Alaska Native† | 24.3* | 22.3 | 20.5 | 21.6* | |||
| Hispanic | 23.2* | 20.6* | 21.6* | 21.2* |
*Average annual percent change is statistically significant (P < .05).
†Data based on Indian Health Service Contract Health Service Delivery Areas (CHSDA). Incidence rates exclude data from Kansas.
Notes: Trends analyzed from 2002 to 2011 using the Joinpoint Regression Program, version 4.1.1, allowing up to 2 joinpoints. Incidence trends based on44 states, representing 92% of the US population.
for the prevention and early detection of cervical cancer. A similarly dramatic decline occurred for stomach cancer, which accounted for 30% and 20% of male and female cancer deaths, respectively, in the 1930s, but just 2% for each in 2011. Although reasons for the decline in the United States and most other parts of the world are complex and not completely understood, contributors are thought to include a lower prevalence of Helicobacter pylori because of improved hygiene and lower salt intake and a higher consumption of fresh fruits and vegetables because of advances in food preservation techniques (eg, refrigeration).46 Recent studies indicate that incidence rates for certain subtypes of stomach cancer are increasing for some subsets of the US population.47,48
During the most recent 5 years for which data are available, the average annual decline in cancer death rates was slightly larger among men (1.8%) than women (1.4%) (Table 5). These declines are driven by continued decreases in death rates for the 4 major cancer sites (lung, breast, prostate, and colorectum). Lung cancer death rates declined 36% between 1990 and 2011 among males and 11% between 2002 and 2011 among females due to reduced tobacco use as a result of increased awareness of the health hazards of smoking and the implementation of comprehensive tobacco control.7,49 Researchers recently estimated that tobacco control efforts adopted in the wake of the first Surgeon General’s report on smoking and health in 1964 have resulted in 8 million fewer premature smoking-related deaths, one-third of which are due to cancer.50,51 Death rates for female breast cancer are down 35% from peak rates, and those from prostate and colorectal cancers are each down 47% as a result of improvements in early detection and treatments.7,29,52,53
In contrast to declining trends for the major cancers, joinpoint analysis indicates that death rates are rising in both sexes for cancers of the oropharynx, anus, liver, pancreas, and soft tissue (including the heart).7 Death rates are also increasing for tonsil cancer and melanoma in men and for uterine cancer in women. Thyroid cancer death rates also increased, but only slightly, from 0.51 (per 100,000 population) in 2007 to 0.52 in 2011 among men and from
0.48 to 0.49 among women.
Recorded Number of Deaths in 2011
A total of 2,515,458 deaths were recorded in the United States in 2011, of which 576,691 (23%) were from cancer. Overall, cancer is the second leading cause of death following heart disease, which accounted for 24% of total deaths. However, cancer is expected to overtake heart disease as the leading cause of death within the next several years. In 2011, cancer was the leading cause of death among adults aged 40 to 79 years and was the first or second leading cause of death in every age group among women (Table 8).
Table 9 presents the number of deaths from all cancers combined and from the 5 most common sites for each 20year age group by sex. More cancer deaths occur in men than in women except for those aged 20 to 39 years and 80 years or older. Breast cancer is the leading cause of cancer death in women aged 20 to 59 years, but is replaced by lung cancer in women aged 60 years or older. Among men, leukemia is the leading cause of cancer death for those aged 20 to 39 years, whereas lung cancer ranks first among men aged 40 years or older.
Cancer Occurrence by Race/Ethnicity
Cancer incidence and death rates vary considerably between and within racial and ethnic groups. Of the 5 broadly defined population groups in Table 10, black men have the highest overall cancer incidence and death rates—about double those of Asian/Pacific Islander (API) men, who have the lowest rates. Cancer incidence and death rates are higher among
| LUNG & | NON-HODGKIN | URINARY | |||||
|---|---|---|---|---|---|---|---|
| STATE | ALL CANCERS MALE FEMALE | BREAST FEMALE | COLORECTUM MALE FEMALE | BRONCHUS MALE FEMALE | LYMPHOMA MALE FEMALE | PROSTATE MALE | BLADDER MALE FEMALE |
| Alabama | 568.8 396.5 | 118.4 | 55.6 38.7 | 100.6 54.8 | 19.7 13.7 | 153.7 | 33.4 7.8 |
| Alaska | 501.4 424.1 | 127.3 | 50.9 41.4 | 79.4 59.5 | 21.3 14.9 | 126.0 | 37.5 11.0 |
| Arizona | 432.8 373.5 | 111.6 | 41.1 31.4 | 60.7 47.7 | 18.7 13.6 | 100.9 | 32.7 8.4 |
| Arkansas*† | 552.7 385.1 | 109.8 | 55.2 38.7 | 106.7 60.2 | 21.9 14.8 | 149.6 | 33.7 7.8 |
| California | 499.2 396.3 | 122.4 | 47.9 36.3 | 58.0 43.1 | 23.0 15.6 | 136.4 | 33.1 7.9 |
| Colorado | 490.7 397.2 | 125.3 | 41.8 32.8 | 54.7 44.0 | 22.5 15.9 | 147.6 | 32.8 8.4 |
| Connecticut | 567.4 455.7 | 136.6 | 49.4 37.4 | 74.3 58.2 | 25.3 17.4 | 152.4 | 47.1 12.3 |
| Delaware | 589.5 444.9 | 128.0 | 49.1 37.5 | 86.0 63.4 | 23.4 16.9 | 168.1 | 43.1 11.4 |
| Dist. of Columbia | 579.8 435.7 | 143.4 | 51.2 43.7 | 75.3 47.2 | 21.0 12.9 | 198.2 | 25.1 9.1 |
| Florida | 514.2 400.5 | 114.6 | 46.6 35.4 | 77.4 56.0 | 21.9 15.1 | 128.3 | 35.0 8.6 |
| Georgia | 564.4 407.8 | 123.8 | 50.8 37.6 | 91.0 54.8 | 22.1 14.8 | 161.0 | 34.2 7.9 |
| Hawaii | 477.9 398.1 | 126.0 | 56.5 37.4 | 62.6 38.4 | 21.3 14.4 | 113.9 | 24.5 6.1 |
| Idaho | 526.2 411.2 | 118.8 | 44.9 34.5 | 61.2 47.1 | 22.5 17.0 | 155.0 | 38.7 9.0 |
| Illinois | 560.6 441.3 | 127.4 | 57.2 41.9 | 84.9 60.4 | 23.9 16.6 | 149.4 | 39.3 9.8 |
| Indiana | 522.5 424.5 | 118.5 | 52.9 41.1 | 95.0 62.9 | 23.5 16.8 | 117.4 | 35.9 8.8 |
| Iowa | 552.1 438.9 | 124.8 | 55.8 42.1 | 83.0 54.7 | 27.0 18.7 | 133.3 | 41.1 8.7 |
| Kansas | 552.5 424.7 | 122.5 | 52.4 38.5 | 78.2 54.0 | 23.6 16.3 | 152.6 | 38.7 9.3 |
| Kentucky | 604.0 464.2 | 120.7 | 62.4 45.0 | 122.9 80.7 | 24.9 17.2 | 128.8 | 40.4 9.8 |
| Louisiana | 601.6 416.6 | 121.3 | 60.8 43.5 | 96.9 57.0 | 24.3 16.6 | 168.9 | 34.3 8.1 |
| Maine | 563.6 454.9 | 126.4 | 48.4 39.3 | 88.1 66.2 | 25.3 17.5 | 133.9 | 48.1 13.0 |
| Maryland | 526.8 420.7 | 130.3 | 46.2 35.9 | 72.2 54.9 | 21.5 15.2 | 152.1 | 33.7 9.2 |
| Massachusetts | 558.7 460.0 | 135.6 | 47.6 37.6 | 77.1 63.6 | 24.8 16.4 | 148.9 | 42.8 11.9 |
| Michigan | 567.4 432.3 | 120.7 | 48.9 37.5 | 83.6 61.2 | 24.6 17.4 | 161.5 | 41.2 10.6 |
| Minnesota‡ | -- | - | -- | -- | -- | - | -- |
| Mississippi | 593.4 402.7 | 116.0 | 60.3 44.0 | 110.2 56.8 | 21.3 14.6 | 161.4 | 30.7 7.3 |
| Missouri | 519.8 423.3 | 122.6 | 53.2 39.4 | 93.0 63.7 | 22.1 15.9 | 121.8 | 34.0 8.5 |
| Montana | 519.6 425.3 | 125.8 | 48.6 38.5 | 68.8 54.7 | 23.0 15.3 | 147.2 | 37.6 10.1 |
| Nebraska | 513.6 421.4 | 121.8 | 54.9 42.9 | 72.2 50.8 | 23.7 17.8 | 136.6 | 35.0 8.5 |
| Nevada*§ | 494.8 394.5 | 112.7 | 50.2 35.8 | 72.2 61.3 | 19.7 15.0 | 133.9 | 36.8 10.6 |
| New Hampshire | 573.2 454.4 | 134.1 | 45.1 38.0 | 78.8 62.8 | 25.3 17.5 | 151.7 | 49.6 13.5 |
| New Jersey | 576.6 450.0 | 129.5 | 52.6 39.9 | 71.4 55.1 | 25.1 17.9 | 166.1 | 42.7 11.4 |
| New Mexico | 447.8 362.2 | 110.0 | 43.0 32.2 | 51.2 37.7 | 17.9 13.4 | 124.4 | 25.7 6.2 |
| New York | 580.6 451.2 | 128.5 | 51.6 39.8 | 75.4 55.6 | 26.4 18.1 | 163.3 | 41.9 10.6 |
| North Carolina | 560.9 417.9 | 126.6 | 48.4 35.7 | 94.4 56.7 | 22.7 15.6 | 149.1 | 36.9 9.0 |
| North Dakota | 524.8 411.1 | 121.8 | 57.2 41.1 | 68.9 44.3 | 23.2 18.5 | 149.0 | 37.8 9.3 |
| Ohio | 531.6 421.6 | 120.0 | 51.8 38.9 | 89.4 59.9 | 22.6 15.6 | 135.8 | 38.5 9.4 |
| Oklahoma | 539.1 414.8 | 120.4 | 51.5 39.5 | 93.5 61.1 | 22.1 16.2 | 142.7 | 34.0 8.2 |
| Oregon | 505.2 429.6 | 129.4 | 44.5 35.3 | 69.1 57.8 | 22.5 15.5 | 134.4 | 37.8 9.5 |
| Pennsylvania | 571.5 456.9 | 126.8 | 54.3 41.1 | 83.2 57.6 | 25.6 17.8 | 145.9 | 44.3 11.1 |
| Rhode Island | 559.0 455.8 | 130.1 | 47.1 38.9 | 82.7 63.1 | 23.3 17.6 | 143.1 | 46.4 14.0 |
| South Carolina | 544.6 402.9 | 123.0 | 48.2 36.7 | 92.5 53.8 | 20.1 13.4 | 146.7 | 31.6 8.5 |
| South Dakota | 501.8 411.7 | 122.0 | 55.9 41.4 | 70.9 49.1 | 22.4 16.3 | 142.0 | 34.2 8.8 |
| Tennessee | 562.5 417.9 | 119.7 | 51.7 38.9 | 101.0 61.4 | 22.4 16.1 | 143.7 | 35.3 8.1 |
| Texas | 504.7 387.1 | 113.7 | 49.7 34.6 | 75.7 47.4 | 22.1 15.6 | 126.9 | 28.8 6.8 |
| Utah | 492.1 361.1 | 112.0 | 38.1 30.4 | 34.2 23.3 | 24.9 15.7 | 170.6 | 31.3 5.6 |
| Vermont | 528.9 441.4 | 129.1 | 43.3 36.1 | 77.2 64.0 | 24.7 17.2 | 133.4 | 39.5 11.1 |
| Virginia | 508.6 398.1 | 125.0 | 45.0 35.1 | 79.7 53.1 | 21.3 14.6 | 143.2 | 33.0 8.3 |
| Washington | 534.9 438.8 | 132.5 | 44.6 35.5 | 70.1 56.1 | 25.9 17.2 | 144.3 | 38.0 9.4 |
| West Virginia | 555.1 437.2 | 110.5 | 57.5 42.5 | 104.7 68.8 | 23.2 16.8 | 126.3 | 39.1 10.8 |
| Wisconsin | 532.9 426.8 | 124.8 | 47.4 37.1 | 73.2 54.1 | 24.7 17.3 | 139.2 | 40.0 10.0 |
| Wyoming | 488.5 387.1 | 112.1 | 44.0 35.5 | 56.3 45.6 | 20.1 14.5 | 143.4 | 37.8 10.6 |
| United States | 535.8 419.1 | 122.8 | 50.0 37.8 | 78.6 54.6 | 23.2 16.1 | 142.1 | 36.7 9.1 |
Rates are per 100,000 and age adjusted to the 2000 US standard population.
*This state’s data are not included in the US combined rates because it did not meet high-quality standards for one or more years during 2007 to 2011 according to the North American Association of Central Cancer Registries (NAACCR).
†Rates are based on incidence data for 2007 to 2009.
‡This state’s registry did not submit cancer incidence data to the NAACCR. §Rates are based on incidence data for 2007 to 2010.
| LUNG & | NON-HODGKIN | ||||||
|---|---|---|---|---|---|---|---|
| STATE | ALL SITES MALE FEMALE | BREAST FEMALE | COLORECTUM MALE FEMALE | BRONCHUS MALE FEMALE | LYMPHOMA MALE FEMALE | PANCREAS MALE FEMALE | PROSTATE MALE |
| Alabama | 251.6 154.3 | 22.9 | 21.5 14.4 | 85.5 40.7 | 8.2 5.2 | 13.3 9.8 | 28.2 |
| Alaska | 215.4 155.0 | 22.7 | 19.6 13.9 | 62.8 45.3 | 8.2 4.7 | 13.4 9.2 | 22.6 |
| Arizona | 182.6 130.0 | 20.1 | 16.5 11.7 | 47.9 32.2 | 7.3 4.8 | 11.3 8.6 | 20.1 |
| Arkansas | 248.7 159.8 | 22.8 | 22.9 15.6 | 88.1 45.3 | 8.3 5.6 | 13.3 9.5 | 24.3 |
| California | 186.8 137.3 | 21.5 | 17.2 12.4 | 45.5 31.5 | 7.7 4.7 | 11.7 9.4 | 21.9 |
| Colorado | 177.7 130.5 | 19.3 | 15.8 12.0 | 42.8 30.3 | 7.4 4.3 | 10.8 9.1 | 22.8 |
| Connecticut | 195.7 141.3 | 20.8 | 15.3 11.4 | 51.3 37.2 | 7.3 4.8 | 13.8 9.9 | 21.5 |
| Delaware | 222.8 158.9 | 22.9 | 19.0 13.5 | 67.3 45.9 | 7.4 4.8 | 12.9 10.1 | 23.6 |
| Dist. of Columbia | 234.8 166.8 | 29.4 | 20.6 18.8 | 57.1 35.4 | 6.5 3.9 | 16.4 12.4 | 37.6 |
| Florida | 200.3 138.8 | 21.0 | 17.6 12.4 | 59.2 38.1 | 7.6 4.6 | 12.0 8.9 | 19.5 |
| Georgia | 222.9 146.3 | 23.1 | 19.8 13.5 | 70.1 38.1 | 7.5 4.3 | 12.3 9.1 | 26.0 |
| Hawaii | 175.8 115.6 | 15.2 | 17.6 10.7 | 46.7 25.5 | 7.4 4.3 | 12.8 9.7 | 15.6 |
| Idaho | 192.2 138.6 | 21.9 | 16.0 12.3 | 48.0 33.9 | 7.8 5.4 | 12.1 8.8 | 25.8 |
| Illinois | 218.9 156.4 | 23.4 | 20.7 14.8 | 64.2 41.6 | 8.3 5.1 | 13.0 10.0 | 23.3 |
| Indiana | 235.8 159.0 | 23.2 | 20.8 14.2 | 77.3 45.5 | 9.1 5.4 | 12.8 9.5 | 22.7 |
| Iowa | 211.1 147.1 | 20.7 | 20.0 14.8 | 63.2 38.1 | 8.8 5.3 | 12.3 8.9 | 21.7 |
| Kansas | 211.3 145.0 | 21.4 | 19.8 13.1 | 64.3 38.8 | 9.2 5.2 | 12.5 9.3 | 20.4 |
| Kentucky | 257.5 172.2 | 22.8 | 22.6 16.1 | 94.5 55.5 | 8.6 5.8 | 12.9 9.5 | 22.3 |
| Louisiana | 250.7 162.2 | 25.0 | 23.3 15.4 | 79.1 43.1 | 8.6 5.0 | 14.3 11.4 | 25.1 |
| Maine | 227.7 156.5 | 20.0 | 19.4 13.7 | 67.6 44.5 | 9.1 5.3 | 12.1 9.9 | 22.1 |
| Maryland | 211.8 150.2 | 23.9 | 19.6 13.2 | 58.9 39.7 | 7.5 4.5 | 13.2 10.1 | 23.7 |
| Massachusetts | 210.8 149.2 | 20.4 | 17.7 12.7 | 58.0 41.2 | 7.7 4.6 | 12.7 10.4 | 21.4 |
| Michigan | 219.4 157.1 | 23.5 | 19.1 13.7 | 66.5 43.5 | 8.9 5.6 | 13.8 10.0 | 21.1 |
| Minnesota | 201.1 143.0 | 20.7 | 17.2 12.1 | 51.9 36.1 | 9.4 5.2 | 12.0 9.2 | 23.4 |
| Mississippi | 264.7 157.0 | 24.2 | 24.6 16.5 | 92.0 41.3 | 8.0 4.6 | 13.8 10.0 | 29.6 |
| Missouri | 225.9 157.8 | 23.8 | 20.9 14.1 | 74.2 45.5 | 8.3 5.3 | 12.9 9.8 | 20.7 |
| Montana | 192.5 142.2 | 20.1 | 15.8 12.7 | 52.3 39.4 | 7.8 4.5 | 11.9 8.0 | 24.8 |
| Nebraska | 204.2 142.5 | 19.8 | 20.4 15.0 | 57.9 35.5 | 8.3 5.5 | 11.3 9.6 | 22.6 |
| Nevada | 206.9 151.7 | 23.5 | 21.0 14.3 | 58.0 45.2 | 6.9 4.4 | 12.8 9.6 | 22.8 |
| New Hampshire | 211.1 152.1 | 21.2 | 16.6 13.3 | 59.2 43.1 | 7.4 4.6 | 13.5 9.9 | 21.4 |
| New Jersey | 203.7 151.0 | 24.6 | 20.2 14.3 | 53.9 36.5 | 7.5 5.0 | 13.6 10.1 | 21.2 |
| New Mexico | 183.8 129.8 | 20.8 | 18.7 12.5 | 42.2 27.9 | 6.2 4.3 | 11.0 8.3 | 23.0 |
| New York | 196.6 143.4 | 22.0 | 18.5 13.3 | 52.9 35.8 | 7.7 4.8 | 12.9 9.9 | 21.4 |
| North Carolina | 227.7 147.2 | 22.7 | 18.8 12.7 | 74.4 39.9 | 7.5 4.8 | 11.8 9.4 | 24.6 |
| North Dakota | 200.0 133.1 | 21.1 | 20.8 13.1 | 52.7 31.4 | 6.7 4.6 | 12.8 8.1 | 22.6 |
| Ohio | 232.8 160.4 | 24.2 | 21.4 14.6 | 72.8 43.9 | 9.2 5.5 | 13.3 10.1 | 23.2 |
| Oklahoma | 238.2 159.7 | 23.5 | 22.1 14.3 | 78.4 46.2 | 8.8 5.6 | 12.3 9.2 | 23.1 |
| Oregon | 206.6 151.4 | 21.1 | 18.2 13.3 | 56.4 41.8 | 8.4 5.0 | 12.3 9.8 | 23.9 |
| Pennsylvania | 222.2 154.9 | 23.5 | 20.7 14.6 | 63.9 39.3 | 8.9 5.4 | 13.3 10.1 | 22.0 |
| Rhode Island | 217.5 147.5 | 20.6 | 18.1 13.4 | 63.9 42.6 | 7.7 4.2 | 12.3 8.7 | 21.3 |
| South Carolina | 236.1 150.0 | 23.5 | 19.9 13.7 | 74.9 39.0 | 7.7 4.6 | 13.1 10.0 | 26.3 |
| South Dakota | 201.4 143.9 | 21.1 | 18.9 13.6 | 60.0 35.0 | 7.6 5.1 | 10.4 9.7 | 22.1 |
| Tennessee | 251.1 158.1 | 22.7 | 21.7 15.3 | 86.5 45.7 | 8.9 5.1 | 13.1 9.6 | 24.0 |
| Texas | 205.2 139.7 | 21.3 | 19.4 12.8 | 58.6 34.5 | 7.8 4.7 | 11.8 8.9 | 20.4 |
| Utah | 154.6 109.1 | 20.8 | 14.0 10.3 | 26.5 16.2 | 7.3 4.6 | 10.3 8.0 | 24.6 |
| Vermont | 213.6 153.2 | 19.7 | 16.8 14.5 | 61.3 45.4 | 8.3 4.7 | 12.9 9.7 | 22.4 |
| Virginia | 216.7 149.1 | 23.5 | 18.3 13.5 | 64.7 39.1 | 8.2 4.7 | 12.7 9.6 | 23.9 |
| Washington | 205.7 149.7 | 21.1 | 16.7 12.6 | 55.6 41.0 | 8.6 5.1 | 12.8 10.1 | 23.4 |
| West Virginia | 246.1 167.8 | 22.5 | 23.7 15.6 | 82.3 49.8 | 8.4 6.2 | 11.9 7.8 | 20.7 |
| Wisconsin | 212.6 148.4 | 21.0 | 17.9 12.4 | 57.8 38.6 | 8.7 5.4 | 13.0 9.8 | 24.3 |
| Wyoming | 192.3 143.4 | 21.1 | 19.1 12.8 | 48.9 34.6 | 7.3 5.3 | 11.9 8.5 | 21.3 |
| United States | 211.6 147.4 | 22.2 | 19.1 13.5 | 61.6 38.5 | 8.1 5.0 | 12.5 9.6 | 22.3 |
Rates are per 100,000 and age adjusted to the 2000 US standard population.
| black than white men for every site included in Table 10 with the exception of kidney cancer mortality, for which rates are similar. The largest disparities are for stomach and prostate cancers, for which death rates in black men are about 2.5 | times those in white men. Factors known to contribute to racial disparities vary by cancer site and include differences in risk factor prevalence and access to high-quality health care, including cancer prevention and early detection, timely | |
|---|---|---|
| VOLUME 00 _ NUMBER 00 _ MONTH 2015 | 21 | |
| 1975 TO | 1978 TO | 1981 TO | 1984 TO | 1987 TO | 1990 TO | 1993 TO | 1996 TO | 1999 TO | 2004 TO | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1977 | 1980 | 1983 | 1986 | 1989 | 1992 | 1995 | 1998 | 2003 | 2010 | |
| All sites | 58 | 62 | 67 | 68 | 72 | 76 | 77 | 79 | 81 | 83† |
| Acute lymphocytic leukemia | 57 | 66 | 71 | 72 | 78 | 83 | 84 | 87 | 90 | 92† |
| Acute myeloid leukemia | 19 | 26 | 27‡ | 31‡ | 37‡ | 42 | 41‡ | 49 | 58 | 66† |
| Bones & joints | 50‡ | 48 | 57‡ | 57‡ | 67‡ | 67 | 74 | 70 | 71 | 79† |
| Brain & other nervous system | 57 | 58 | 57 | 62 | 64 | 64 | 71 | 75 | 74 | 74 |
| Hodgkin lymphoma | 81 | 87 | 88 | 90 | 87 | 97 | 95 | 96 | 95 | 98† |
| Neuroblastoma | 53 | 57 | 55 | 52 | 63 | 76 | 67 | 66 | 72 | 77† |
| Non-Hodgkin lymphoma | 43 | 53 | 67 | 70 | 71 | 77 | 81 | 83 | 90 | 86† |
| Soft tissue | 61 | 74 | 69 | 73 | 66 | 80 | 77 | 71 | 79 | 81† |
| Wilms tumor | 73 | 79 | 87 | 91 | 92 | 92 | 92 | 92 | 92 | 92† |
*Survival rates are adjusted for normal life expectancy and are based on follow-up of patients through 2011.
†The difference in rates between 1975 to 1977 and 2004 to 2010 is statistically significant (P < .05).
‡The standard error of the survival rate is between 5 and 10 percentage points.
54,55
diagnosis, and optimal treatment.Even among Medicare-insured patients, blacks are less likely than whites to receive standard-cancer therapies for lung, breast, colorectal, and prostate cancers. 56 A major source of these inequalities is the disproportionately high burden of poverty in the black community. According to the US Census Bureau, 27% of blacks lived in poverty and 19% were without health insurance in 2012, compared with 10% and 11%, respectively, of non-Hispanic whites.57
Higher mortality rates among blacks compared with whites partly reflect a later stage of disease at diagnosis. This disparity is particularly striking for cancers of the uterine corpus, oral cavity, female breast, and cervix (Fig. 6). Moreover, black patients have lower stage-specific survival for most cancer types (Fig. 7). As a result, although black women have a lower breast cancer incidence rate than white women, they have a higher breast cancer death rate (Table 10). The higher incidence rate among white women is thought to reflect a combination of factors that affect both diagnosis (more prevalent mammography) and underlying disease occurrence (such as later age at first birth and greater use of menopausal hormone therapy).58 The higher risk of death from breast cancer among black women is thought to reflect a higher prevalence of comorbidities, a longer time to follow-up after an abnormal mammogram, less receipt of high-quality treatment, and a higher prevalence of aggressive tumor characteristics.59–61 However, an analysis of clinical trial data showed that black women were less likely than white women to survive their breast cancer despite uniform treatment, even after controlling for stage of disease, tumor characteristics, follow-up, and socioeconomic status.62
Cancer incidence and death rates are lower among APIs, American Indians/Alaska Natives (AI/ANs), and Hispanics than non-Hispanic whites for all cancer sites combined and for the 4 most common cancer sites. However, cancers associated with infectious agents (eg, those of the uterine cervix, stomach, and liver) are generally more common in nonwhite populations. For example, stomach and liver cancer incidence and death rates are twice as high in the API population as in whites, reflecting a higher prevalence of chronic infection with Helicobacter pylori and hepatitis B virus, respectively, in immigrant countries of origin.63 Kidney cancer incidence and death rates are the highest among AI/ANs, which may be due in part to high rates of obesity, smoking, and hypertension in this population. Regional variation in the prevalence of these risk factors may contribute to striking geographic differences in kidney cancer death rates among AI/AN men, which are highest in the Southern and Northern Plains and lowest in the East and Pacific Coast.64
Table 11 shows the variation in trends in cancer incidence and death rates during the most recent 5 data years by race and ethnicity. These trends are based on incidence data from 2002 to 2011 covering 92% of the US population, but are not adjusted for reporting delays. Among men, the magnitude of decline for incidence rates is larger than that for death rates, while the opposite is generally true for women. Significant declines in incidence rates in women were confined to blacks (0.4% per year) and Hispanics (0.6% per year). Black men continue to have the largest decline in death rates (2.5% per year).
Regional Variations in Cancer Rates
Tables 12 and 13 depict current cancer incidence and death rates for selected cancers by state. The largest geographic variation in cancer occurrence by far is for lung cancer, reflecting the large historical and continuing differences in smoking prevalence among states.49 For example, lung cancer incidence rates in Kentucky, which has historically had the highest smoking prevalence, are
3.5 times higher than those in Utah, which has the lowest smoking prevalence. There is a 2-fold difference for prostate cancer incidence rates, which range from 100.9 (per 100,000 population) in Arizona to 198.2 in the District of Columbia, likely reflecting both state differences in PSA testing prevalence and population demographics.26 In contrast, state variations for other cancer types are smaller in both absolute and relative terms. For example, breast cancer incidence rates range from 109.8 (per 100,000 population) in Arkansas to 143.4 in the District of Columbia, arelativedifferenceofjust23%.Someofthisvariation is attributable to differences in mammography prevalence.65 State variation in cancer incidence rates reflects differences in the use of screening tests and diagnostic practices in addition to differences in the prevalence of risk factors, while the variation in death rates reflects differences in cancer occurrence and survival.
Cancer in Children
Cancer is the second most common cause of death among children aged 1 to 14 years in the United States, surpassed only by accidents. In 2015, an estimated 10,380 children (0-14 years) will be diagnosed with cancer (excluding benign/borderline brain tumors) and 1,250 will die from the disease. Benign and borderline brain tumors are not included in the estimated new cases for 2015 because the calculation method requires historic data and these tumors were not reportable until 2004. Leukemia (77% of which are lymphoid leukemias) accounts for 30% of all childhood cancers (including benign brain tumors). Cancers of the brain and other nervous system are the second most common cancer type (26%), followed by neuroblastoma (6%), soft tissue sarcomas (6%, one-half of which are rhabdomyosarcoma), renal (Wilms) tumors (5%), non-Hodgkin lymphomas (including Burkitt lymphoma) (5%), and Hodgkin lymphomas (3%).8
Cancers in adolescents (aged 15-19 years) differ somewhat from those in children in terms of type and distribution. For example, a smaller proportion of the cancers diagnosed in adolescents are leukemias and a larger proportion are lymphomas. Cancers of the brain and other nervous system are most common (20%), followed by leukemia (13%), Hodgkin lymphoma (13%), thyroid carcinoma (10%), and gonadal germ cell tumors (9%). Melanoma accounts for 5% of the cancers diagnosed in this age group.
From 2007 to 2011, the overall incidence rate for cancer increased by 0.6% per year in children and was stable in adolescents. In contrast, death rates have been declining for decades. From 1970 to 2011, the death rate for childhood cancer decreased 67% (from 6.3 to 2.1 per 100,000 population) and the death rate for adolescents decreased by 58% (from 7.2 to 3.0). Table 14 provides trends in survival rates for the most common childhood cancers. The 5-year relative survival rate for all cancer sites combined improved from 58% for children diagnosed during 1975-1977 to 83% for those diagnosed during 2004-2010. The substantial progress for all of the major childhood cancers reflects both improvements in treatment and high levels of participation in clinical trials.
Limitations
The projected numbers of cancer cases and deaths in 2015 should be interpreted with caution because they are model-based estimates that may vary considerably from year to year for reasons other than changes in cancer occurrence. For instance, estimates are affected by changes in method, which are implemented regularly as modeling techniques improve and surveillance coverage becomes more complete. In addition, the model is sometimes oversensitive or under-sensitive to abrupt or large changes in observed data. Therefore, while these estimates provide a reasonably accurate portrayal of the contemporary cancer burden, they should not be used to track cancer occurrence over time. Age-standardized or age-specific cancer death rates from the NCHS and cancer incidence rates from SEER, NPCR, and/or NAACCR are the most informative indicators of cancer trends.
Errors in reporting race/ethnicity in medical records and on death certificates may result in underestimates of cancer incidence and mortality rates in nonwhite and nonblack populations. This is particularly relevant for AI/AN populations. It is also important to note that cancer data in the United States are primarily reported for broad racial and ethnic groups that are not homogenous, masking important differences in the cancer burden within these groups.
Conclusions
Cancer death rates have been continuously declining for the past 2 decades. Overall, the risk of dying from cancer decreased by 22% between 1991 and 2011. Regionally, progress has been most rapid for residents of the Northeast, among whom death rates have declined by 25% to 30%, and slowest in the South, where rates declined by about 15%. Further reductions in cancer death rates can be accelerated by applying existing cancer control knowledge across all segments of the population, with an emphasis on those in the lowest socioeconomic bracket and other disadvantaged populations. �
References
- Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Mortality-All COD, Aggregated With State, Total US (1969-2011) <Katrina/Rita Population Adjustment>. Bethesda, MD: National Cancer Institute, Division of Cancer Control and Population Sciences, Surveillance Research Program, Cancer Statistics Branch; 2014; underlying mortality data provided by National Center for Health Statistics 2014.
- Wingo PA, Cardinez CJ, Landis SH, et al. Long-term trends in cancer mortality in the United States, 1930-1998. Cancer. 2003; 97(suppl 12):3133-3275.
- Murphy SL, Xu J, Kochanek KD. Deaths: Final Data for 2010. National Vital Statistics Reports. Vol 64. No. 4. Hyattsville, MD: National Center for Health Statistics; 2013.
- Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence-SEER 9 Regs Research Data, Nov. 2013 Sub (1973-2011) <Katrina/Rita Population Adjustment>Linked To County Attributes-Total US, 1969-2012 Counties. Bethesda, MD: National Cancer Institute, Division of Cancer Control and Population Sciences, Surveillance Research Program, Surveillance Systems Branch; 2014.
- Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence-SEER 13 Regs Research Data, Nov. 2013 Sub (1992-2011) <Katrina/Rita Population Adjustment>Linked To County Attributes-Total US, 1969-2012 Counties. Bethesda, MD: National Cancer Institute, Division of Cancer Control and Population Sciences, Surveillance Research Program, Surveillance Systems Branch; 2014.
- Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence-SEER 18 Regs Research Data 1 Hurricane Katrina Impacted Louisiana Cases, Nov. 2013 Sub (2000-2011) <Katrina/Rita Population Adjustment>Linked To County Attributes-Total US, 1969-2012 Counties. Bethesda, MD: National Cancer Institute, Division of Cancer Control and Population Sciences, Surveillance Research Program, Surveillance Systems Branch; 2014.
- Howlader N, Noone AM, Krapcho M, et al, eds. SEER Cancer Statistics Review, 19752011. Bethesda, MD: National Cancer Institute; 2014.
- Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: North American Association of Central Cancer Registries (NAACCR) Incidence-CiNA Analytic File, 1995-2011, for Expanded Races, Custom File With County, ACS Facts and Figures Projection Project, North American Association of Central Cancer Registries. Bethesda, MD: National Cancer Institute, Division of Cancer Control and Population Sciences, Surveillance Research Program, Surveillance Systems Branch; 2014.
- Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: North American Association of Central Cancer Registries (NAACCR) Incidence-CiNA Analytic File, 1995-2011, for NHIAv2 Origin, Custom File With County, ACS Facts and Figures Projection Project, North American Association of Central Cancer Registries. Bethesda, MD: National Cancer
Institute, Division of Cancer Control and Population Sciences, Surveillance Research Program, Surveillance Systems Branch; 2014.
- Copeland G, Lake A, Firth R, et al. Cancer in North America: 2007-2011. Vol 1. Combined Cancer Incidence for the United States, Canada and North America. Springfield, IL: North American Association of Central Cancer Registries Inc; 2014.
- Copeland G, Lake A, Firth R, et al. Cancer in North America: 2007-2011. Vol 2. Registry-Specific Cancer Incidence in the United States and Canada. Springfield, IL: North American Association of Central Cancer Registries Inc; 2014.
- Fritz A, Percy C, Jack A, et al. International Classification of Diseases for Oncology. 3rd ed. Geneva: World Health Organization; 2000.
- Statistical Research and Applications Branch. DevCan: Probability of Developing or Dying of Cancer Software. Version 6.7.1. Bethesda, MD: Statistical Research and Applications Branch, National Cancer Institute; 2005.
- Surveillance Research Program, National Cancer Institute. SEER*Stat Software. Version 8.1.5. Bethesda, MD: National Cancer Institute; 2014.
- Joinpoint Regression Program, Version
- 4.1.1. Bethesda, MD: Statistical Research and Applications Branch, National Cancer Institute; 2014.
- Clegg LX, Feuer EJ, Midthune DN, Fay MP, Hankey BF. Impact of reporting delay and reporting error on cancer incidence rates and trends. J Natl Cancer Inst. 2002;94: 1537-1545.
- Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence-SEER 13 Regs Research Data (with SEER Delay Factors), Nov. 2013 Sub (1992-2011) <Katrina/Rita Population Adjustment>-Linked To County Attributes-Total US, 1969-2012 Counties. Bethesda, MD: National Cancer Institute, Division of Cancer Control and Population Sciences, Surveillance Research Program, Surveillance Systems Branch; 2014.
- Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence-SEER 9 Regs Research Data (with SEER Delay Factors), Nov. 2013 Sub (1973-2011) <Katrina/Rita Population Adjustment>-Linked To County Attributes-Total US, 1969-2012 Counties. Bethesda, MD: National Cancer Institute, Division of Cancer Control and Population Sciences, Surveillance Research Program, Surveillance Systems Branch; 2014.
- Pickle LW, Hao Y, Jemal A, et al. A new method of estimating United States and state-level cancer incidence counts for the current calendar year. CA Cancer J Clin. 2007;57:30-42.
- Zhu L, Pickle LW, Ghosh K, et al. Predicting US-and state-level cancer counts for the current calendar year: Part II: evaluation of spatiotemporal projection methods for incidence. Cancer. 2012;118:1100-1109.
- National Cancer Institute. Cancer Query System: Delay-Adjusted SEER Incidence Factors. surveillance.cancer.gov/delay/can ques.html . Accessed October 6, 2014.
- Chen HS, Portier K, Ghosh K, et al. Predicting US-and state-level cancer counts for the
current calendar year: Part I: evaluation of temporal projection methods for mortality. Cancer. 2012;118:1091-1099.
- Kabat GC, Anderson ML, Heo M, et al. Adult stature and risk of cancer at different anatomic sites in a cohort of postmenopausal women. Cancer Epidemiol Biomarkers Prev. 2013;22:1353-1363.
- Walter RB, Brasky TM, Buckley SA, Potter JD, White E. Height as an explanatory factor for sex differences in human cancer. J Natl Cancer Inst. 2013;105:860-868.
- Potosky AL, Kessler L, Gridley G, Brown CC, Horm JW. Rise in prostatic cancer incidence associated with increased use of transurethral resection. J Natl Cancer Inst. 1990;82:1624-1628.
- Potosky AL, Miller BA, Albertsen PC, Kramer BS. The role of increasing detection in the rising incidence of prostate cancer. JAMA. 1995;273:548-552.
- Holford TR, Cronin KA, Mariotto AB, Feuer EJ. Changing patterns in breast cancer incidence trends. J Natl Cancer Inst Monogr. 2006;(36):19-25.
- Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335-351.
- Edwards BK, Ward E, Kohler BA, et al. Annual report to the nation on the status of cancer, 1975-2006, featuring colorectal cancer trends and impact of interventions (risk factors, screening, and treatment) to reduce future rates. Cancer. 2010;116:544-573.
- Cress RD, Morris C, Ellison GL, Goodman MT. Secular changes in colorectal cancer incidence by subsite, stage at diagnosis, and race/ethnicity, 1992-2001. Cancer. 2006;107(suppl 5):1142-1152.
- Siegel RL, Ward EM, Jemal A. Trends in colorectal cancer incidence rates in the United States by tumor location and stage, 1992-2008. Cancer Epidemiol Biomarkers Prev. 2012;21:411-416.
- Centers for Disease Control and Prevention, National Center for Health Statistics. National Health Interview Surveys, 2000, 2013. Public use data files, 2001, 2014.
- Harris JE. Cigarette smoking among successive birth cohorts of men and women in the United States during 1900-80. J Natl Cancer Inst. 1983;71:473-479.
- Jemal A, Ma J, Rosenberg PS, Siegel R, Anderson WF. Increasing lung cancer death rates among young women in southern and midwestern States. J Clin Oncol. 2012;30: 2739-2744.
- Legler JM, Feuer EJ, Potosky AL, Merrill RM, Kramer BS. The role of prostate-specific antigen (PSA) testing patterns in the recent prostate cancer incidence decline in the United States. Cancer Causes Control. 1998;9:519-527.
- Draisma G, Etzioni R, Tsodikov A, et al. Lead time and overdiagnosis in prostate-specific antigen screening: importance of methods and context. J Natl Cancer Inst. 2009;101:374-383.
- Howard DH, Tangka FK, Guy GP, Ekwueme DU, Lipscomb J. Prostate cancer screening in men ages 75 and older fell by 8 percentage points after Task Force recommendation. Health Aff (Millwood). 2013; 32:596-602.
- Drazer MW, Prasad SM, Huo D, et al. National trends in prostate cancer screening among older American men with limited 9year life expectancies: evidence of an increased need for shared decision making. Cancer. 2014;120:1491-1498.
- Li J, German R, King J, et al. Recent trends in prostate cancer testing and incidence among men under age of 50. Cancer Epidemiol. 2012;36:122-127.
- Ferdinand R, Mitchell SA, Batson S, Tumur
- I. Treatments for chronic myeloid leukemia: a qualitative systematic review. J Blood Med. 2012;3:51-76.
- Pinsky PF, Church TR, Izmirlian G, Kramer BS. The National Lung Screening Trial: results stratified by demographics, smoking history, and lung cancer histology. Cancer. 2013;119:3976–3983.
- National Lung Screening Trial Research Team, Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med. 2011;365:395-409.
- Welch HG, Schwartz LM, Woloshin S. Are increasing 5-year survival rates evidence of success against cancer? JAMA. 2000;283: 2975-2978.
- Ezzati M, Friedman AB, Kulkarni SC, Murray CJ. The reversal of fortunes: trends in county mortality and cross-county mortality disparities in the United States. PLoS Med. 2008;5:e66.
- Grauman DJ, Tarone RE, Devesa SS, Fraumeni JF Jr. Alternate ranging methods for cancer mortality maps. J Natl Cancer Inst. 2000;92:534-543.
- Bertuccio P, Chatenoud L, Levi F, et al. Recent patterns in gastric cancer: a global overview. Int J Cancer. 2009;125: 666-673.
- Anderson WF, Camargo MC, Fraumeni JF Jr, Correa P, Rosenberg PS, Rabkin CS. Age-specific trends in incidence of noncar
dia gastric cancer in US adults. JAMA. 2010;303:1723-1728.
- Camargo MC, Anderson WF, King JB, et al. Divergent trends for gastric cancer incidence by anatomical subsite in US adults. Gut. 2011;60:1644-1649.
- Jemal A, Thun MJ, Ries LA, et al. Annual report to the nation on the status of cancer, 1975-2005, featuring trends in lung cancer, tobacco use, and tobacco control. J Natl Cancer Inst. 2008;100:1672-1694.
- Holford TR, Meza R, Warner KE, et al. Tobacco control and the reduction in smoking-related premature deaths in the United States, 1964-2012. JAMA. 2014;311: 164-171.
- US Department of Health and Human Services. The Health Consequences of Smoking-50 YearsofProgress. A Reportofthe Surgeon General. Atlanta, GA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014.
- Berry DA, Cronin KA, Plevritis SK, et al; Cancer Intervention and Surveillance Modeling Network (CISNET) Collaborators. Effect of screening and adjuvant therapy on mortality from breast cancer. N Engl J Med. 2005;353:1784-1792.
- Etzioni R, Tsodikov A, Mariotto A, et al. Quantifying the role of PSA screening in the US prostate cancer mortality decline. Cancer Causes Control. 2008;19:175-181.
- Ward E, JemalA,CokkinidesV,et al. Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin. 2004;54:78-93.
- Bach PB, Schrag D, Brawley OW, Galaznik A, Yakren S, Begg CB. Survival of blacks and whites after a cancer diagnosis. JAMA. 2002;287:2106-2113.
- Gross CP, Smith BD, Wolf E, Andersen M. Racial disparities in cancer therapy: did the
gap narrow between 1992 and 2002? Cancer. 2008;112:900-908.
- DeNavas-Walt C, Proctor BD, Smith JC. US Census Bureau, Current Population Reports, P60-245. Income, Poverty, and Health Insurance Coverage in the United States: 2012. Washington, DC: US Government Printing Office; 2013.
- Ghafoor A, Jemal A, Ward E, Cokkinides V, Smith R, Thun M. Trends in breast cancer by race and ethnicity. CA Cancer J Clin. 2003;53:342-355.
- Menashe I, Anderson WF, Jatoi I, Rosenberg PS. Underlying causes of the black-white racial disparity in breast cancer mortality: a population-based analysis. J Natl Cancer Inst. 2009;101:993-1000.
- Press R, Carrasquillo O, Sciacca RR, Giardina EG. Racial/ethnic disparities in time to follow-up after an abnormal mammogram. J Womens Health (Larchmt). 2008;17:923-930.
- Tammemagi CM, Nerenz D, Neslund-Dudas C, Feldkamp C, Nathanson D. Comorbidity and survival disparities among black and white patients with breast cancer. JAMA. 2005;294:1765-1772.
- Albain KS, Unger JM, Crowley JJ, Coltman CA Jr, Hershman DL. Racial disparities in cancer survival among randomized clinical trials patients of the Southwest Oncology Group. J Natl Cancer Inst. 2009;101:984-992.
- Parkin DM. The global health burden of infection-associated cancers in the year 2002. Int J Cancer. 2006;118:3030-3044.
- White MC, Espey DK, Swan J, Wiggins CL, Eheman C, Kaur JS. Disparities in cancer mortality and incidence among American Indians and Alaska Natives in the United States. Am J Public Health. 2014;104(suppl 3):S377-S387.
- DeSantis C, Siegel R, Bandi P, Jemal A. Breast cancer statistics, 2011. CA Cancer J Clin. 2011;61:409-418.